Triple drug regimen proven effective against non-structural protein-1 of SARS-CoV-2
In a recent preprint study posted to Research Square* and currently under consideration at Scientific Reports, researchers evaluated the synergistic activity of drugs acting against non-structural protein 1 (Nsp1) of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) to decrease the viral infectivity.

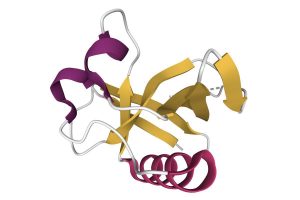
Nsp1 is the first SARS-CoV-2 protein expressed upon viral entry into host cells. Although Nsp1 activity suppresses host protein synthesis, the viral protein synthesis remains unhindered. Nsp1 also inhibits the production of interferons-1 and 3 (IF-1 and IF-3) which are essential mediators of innate humoral immune mechanisms.
Additionally, Nsp1 is the only SARS-CoV-2 protein that gives rise to substantial apoptotic cell death. Thus, therapies targeted against Nsp1 could reduce viral infectivity, slow down viral replication, and decrease the clinical severity of coronavirus disease 2019 (COVID-19). Anti-Nsp1 therapy could be effective against all SARS-CoV-2 strains, since the Nsp1 protein sequence is the same across all viral strains.
Although vaccines have been developed globally for protection against COVID-19, their efficacy may be decreased due to immune antibody evasive properties of SARS-CoV-2 strains. Thus, there is an urgent need for therapeutic interventions targeted against SARS-CoV-2 proteins, such as Nsp1, to reduce COVID-19-associated morbidity and mortality.
About the study
The researchers conducted a cytopathic multiplex assay in cultured lung cells belonging to the H1299 cell line for the identification of drugs with potent anti-Nsp1 action. The detection of such drugs was based on the apoptotic property of Nsp1.
In silico virtual screening of drug libraries was performed to classify drug molecules based on their binding affinity against two main sites of Nsp1: the C-terminal helix-loop-helix site and the RNA-binding groove. Databases such as DrugBank, PubChem, ZINC15, and eDrug-3D were used to identify the necessary drugs.
An artificial gene that encoded Nsp1 was created using genomic sequences of the original Wuhan-SARS-CoV-2 strain. Messenger ribonucleic acid (mRNA) obtained from the virus was subjected to transcription for adequate Nsp1 expression in the cultured pulmonary cells. Subsequently, mRNA transfection was performed using the mRNA lipofection technique. A day post-transfection, apoptosis was observed easily in phase-contrast pictures of the cultured H1299 cells.
Three measures of cell viability – metabolism, mitochondrial membrane integrity, and cell adherence – were grouped together and quantified using fluorescent dyes to devise the viability index for the quantitative measurement of Nsp1 activity. Drug efficacy was measured in terms of EC100 (concentrations at which the maximum efficacy was demonstrated). The half-maximal cytotoxic concentration (CC50) was also determined with help of the viability index. A ratio of CC50/EC100 was calculated to derive the safety index of the drugs.
Results and discussion
Although no single drug could completely reverse Nsp1 action independently, a triple-drug regimen of Montelukast, Ponatinib, and Rilpivirine (MPR) at concentrations of 0.625 µM, 0.05 µM, and 0.025 µM, respectively, significantly reduced Nsp1-mediated apoptotic death equivalent to Nsp1 gene null mutation effects. These nanomolar concentrations are also clinically achievable in humans. The independent efficacy of the drugs was less than 20% but increased to 59% when used in combination, equivalent to null mutations (Mut) E and D. The CC50 value and safety index of the MPR regimen were 8X and 16, respectively. In addition, all these drugs could be orally administered and have been tested priorly in human beings with known adverse effects. The anti-Nsp1 MPR efficacy could be due to drug binding to the RNA groove of Nsp1.
Other drugs such as Tirilazad and Pazopanib were also tested but could not be effectively used clinically. Although Tirilazad was tightly bound to the Nsp1 RNA groove and significantly increased efficacy when combined with Montelukast or Ponatinib, 1-5 µM of Tirilazad was required to achieve the desired results. The drug also had limited bioavailability and was an investigational drug, which was a barrier to the clinical translation of the drug.
Although Pazopanib demonstrated the highest binding affinity for the Nsp1 helix-loop-helix area, 80 µM of Pazopanib was required to achieve efficacy similar to the effect of null mutations. This limitation precluded clinical usage of Pazopanib. Thus, Rilpivirine, which had the next highest binding affinity for the Nsp1 helix-loop-helix, was used.
Conclusion
The study findings showed that a triple-drug combination of MPR effectively inhibited Nsp1 activity in cultured lung cells. Since these combinational drugs have been previously used in humans, much information is already known regarding their potential side effects.
Additionally, their oral route of administration also facilitates their clinical use. Thus, the MPR drug combination could provide an effective orally administered substitute to parenterally administered vaccines for the reduction of SARS-CoV-2 virulence.
*Important notice
Research Square publish preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Hung-The Kao, Andrew Orry, Michael Palfreyman, Barbara Porton. (2022). Synergistic Interactions of Repurposed Drugs that Inhibit Nsp1, a Major Virulence Factor for COVID-19. Scientific reports. doi: https://doi.org/10.21203/rs.3.rs-1362548/v1 https://www.researchsquare.com/article/rs-1362548/v1
Posted in: Medical Research News | Medical Condition News | Disease/Infection News
Tags: Antibody, Apoptosis, Assay, binding affinity, Cell, Cell Death, Cell Line, Coronavirus, Coronavirus Disease COVID-19, covid-19, Drugs, Efficacy, Fluorescent Dyes, Gene, Genomic, Helix, Interferons, Membrane, Metabolism, Mortality, Mutation, Pazopanib, Protein, Protein Synthesis, Research, Respiratory, Ribonucleic Acid, RNA, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Structural Protein, Syndrome, Transcription, Transfection, Translation, Virus

Written by
Pooja Toshniwal Paharia
Dr. based clinical-radiological diagnosis and management of oral lesions and conditions and associated maxillofacial disorders.
Source: Read Full Article