‘Agony of Choice’ for Clinicians Treating Leukemia
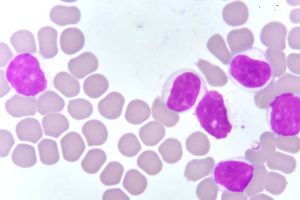
With an abundance of targeted therapies transforming the treatment landscape for chronic lymphocytic leukemia (CLL), picking the optimal drug or drug sequence for the right situation can be a challenge, but emerging data is helping guide clinicians facing the “agony of choice,” a new review reports.
“Targeted therapies have outnumbered chemoimmunotherapy-based treatment approaches, demonstrating superior efficacy and tolerability profiles across nearly all CLL patient subgroups in the frontline and relapsed disease treatment setting,” author Jan-Paul Bohn, MD, PhD, of the department of internal medicine V, hematology and oncology, at Medical University of Innsbruck (Austria), reported in the review published in Memo, the Magazine of European Medical Oncology.
The options leave clinicians “spoilt for choice when selecting optimal therapy,” he said.
The three major drug classes to emerge – inhibitors of Bruton tyrosine kinase (BTK), antiapoptotic protein B-cell lymphoma 2 (BCL2) and phosphoinositide 3′-kinase (PI3K) – all appear similar in efficacy and tolerability.
Particularly in high-risk patients, the drugs have been so effective that the less desirable previous standard of “chemoimmunotherapy has widely faded into the background in the Western hemisphere,” Bohn wrote.
However, with caveats of the newer drugs including acquired resistances and potential toxicities, challenges have shifted to determining how to best juggle and/or combine the agents.
Frontline Therapy
In terms of frontline options for CLL therapy, the BTK inhibitors, along with the BCL2 inhibitor venetoclax have been key in negating the need for chemotherapy, with some of the latest data showing superiority of venetoclax in combination with obinutuzumab (GVe) over chemotherapy even in the higher-risk subset of patients with mutated IGHV status and without TP53 disruption.
Hence, “chemoimmunotherapy may now even be questioned in the remaining subset of CLL patients with mutated IGHV status and without TP53 disruption,” Bohn reported.
That being said, the criteria for treatment choices in the frontline setting among the newer drug classes can often come down to the key issues of patients’ comorbidities and treatment preferences.
For example, in terms of patients who have higher risk because of tumor lysis syndrome (TLS), or issues including declining renal function, continuous BTK inhibitor treatment may be the preferred choice over the combination of venetoclax plus obinutuzumab (GVe), Bohn noted.
Conversely, for patients with cardiac comorbidities or a higher risk of bleeding, the GVe combination may be preferred over ibrutinib, with recent findings showing ibrutinib to be associated with as much as an 18-times higher risk of sudden unexplained death or cardiac death in young and fit patients who had preexisting arterial hypertension and/or a history of cardiac disorders requiring therapy.
For those with cardiac comorbidities, the more selective second-generation BTK inhibitor acalabrutinib is a potentially favorable alternative, as the drug is “at least similarly effective and more favorable in terms of tolerability, compared with ibrutinib, particularly as far as cardiac and bleeding side effects are considered,” Bohn said.
And in higher-risk cases involving TP53 dysfunction, a BTK inhibitor may be superior to GVe for frontline treatment, Bohn noted, with data showing progression-free survival in patients with and without deletion 17p to be significantly reduced with GVe versus the BTK inhibitor ibrutinib.
Relapsed and Refractory Disease
With similarly high efficacy observed with the new drug classes among relapsed and/or refractory patients, chemoimmunotherapy has likewise “become obsolete in nearly all patients naive to novel agents at relapse who typically present with genetically high-risk disease,” Bohn noted.
He wrote that most of the recommendations for frontline therapy hold true in the relapsed and refractory patients, with comorbidities and personal preferences again key drivers of treatment choices.
While data is currently limited regarding benefits of venetoclax-based regimens over BTK inhibitors in relapsed/refractory patients, there is “growing evidence suggesting similar clinical outcomes achievable with these agents in either order,” Bohn wrote.
Further recommendations regarding relapsed or refractory patients include:
-
Among patients who do experience disease progression while on continuous treatment with BTK inhibitors, venetoclax-based regimes seem most effective. However, with relapse after venetoclax-based regimes, some growing evidence supports retreatment with the drug “depending on depth and duration of response achieved after first venetoclax exposure,” Bohn noted.
-
For patients with deletion 17p, venetoclax shows promising efficacy during relapse when given as monotherapy until disease progression or occurrence of unacceptable toxicity.
-
And for patients with TP53 abnormalities, the considerations are the same as for frontline therapy, with venetoclax showing promising efficacy when given in monotherapy until disease progression or occurrence of unacceptable toxicity.
Of note, PI3K inhibitors are generally not used in CLL patients naive to BTK and BCL2 inhibitors because of the higher risk of immune-mediated toxicities and infectious complications associated with the currently approved PI3K inhibitors idelalisib and duvelisib, he reported.
Nevertheless, “PI3K inhibitors remain a valuable therapeutic addition in patients refractory or intolerant to BTK inhibitors and venetoclax-based regimens,” Bohn said.
Newer Agents, Fixed Duration
Commenting on the review, hematologist Seema A. Bhat, MD, an assistant professor with the Ohio State University Comprehensive Cancer Center, Columbus, said that the advances with targeted therapies in CLL are paying off with improved survival.
“With these recent advances in the treatment of CLL, especially the availability of targeted therapies, there has been an improvement in survival of patients with CLL, as the CLL-related death rate steadily reduced by approximately 3% per year between 2006 and 2015,” she said in an interview.
She added that even-newer agents in development, including the reversibly binding BTK inhibitor–like pirtobrutinib and nemtabrutinib, when approved, will further add to the treatment choices for patients.
Meanwhile, a key area of focus is the combination of BTK inhibitors and BCL2 inhibitors, specifically for a fixed duration of time to obtain a deeper response and hence possibility a time-limited therapy, she noted. “We are also excited about the possibility of having more fixed-duration treatments available for our patients, which will make their treatment journey less troublesome, both physically as well as financially.”
Bohn reported receiving personal fees from AbbVie, AstraZeneca and Janssen for advisory board participation. Bhat has served on advisory board for AstraZeneca and received honorarium from them.
This article originally appeared on MDedge.com, part of the Medscape Professional Network.
Source: Read Full Article