Monkeypox: When to get tested and what to do if you’re exposed
On July 23, 2022, the World Health Organization (WHO) declared monkeypox a public health emergency of international concern, calling for a coordinated international response to slow the spread of disease. It is the second time in 2 years that WHO has taken this step, ranking monkeypox amongst two other diseases, COVID-19 and polio, that currently carry the classification. Past outbreaks of influenza A, Ebola, Zika, Middle East respiratory syndrome coronavirus (MERS) and yellow fever have all historically made the list.
On the heels of the declaration came concerning reports of over 20,000 cases of monkeypox in 71 countries where the disease is not endemic. Nearly 5,000 of these confirmed or suspected cases have occurred on U.S. soil, and public health experts are expressing significant concerns about capacity to effectively control the spread of this disease, an especially disheartening assessment in light of recent SARS-CoV-2 experiences.
How do we contain monkeypox outbreaks?
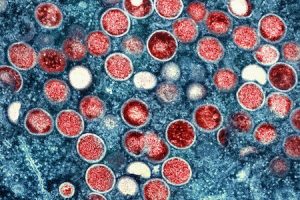
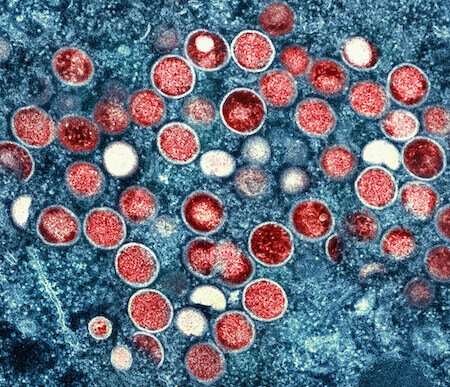
If the early days of the COVID-19 pandemic taught us anything, it’s that timely and accurate diagnosis are critical to our ability to slow transmission of the virus. Unlike SARS-CoV-2, which was a novel virus when it emerged in late 2019, monkeypox virus has been around for a bit. It is a member of the Orthopoxvirus genus and relative of smallpox. The virus was first discovered causing pox-like disease in laboratory monkeys in 1958 and the first case of human infection was reported in 1970. This means that previously developed diagnostic, treatment and prevention strategies are available and expected to benefit current efforts to contain outbreaks.
Yet, a few noteworthy differences between current outbreaks and what has been historically observed in endemic countries have generated important questions about the evolution of the virus, presentation and spread of disease. Public messaging about what to do if one comes in contact with the virus is, therefore, especially critical during this time. How is monkeypox diagnosed? When and where should one get tested? Can vaccines be administered after exposure?
When to get tested for monkeypox
Contact your physician and seek testing if either of the following occurs:
- You have known exposure (have been in close contact) with someone who has been diagnosed with monkeypox.
- You develop symptoms of the disease.
Monkeypox transmission
Monkeypox virus is less transmissible than SARS-CoV-2, as it is primarily spread through direct person-to-person contact, either via respiratory droplets or exposure to infectious lesions or other bodily fluids. The virus is not known to linger in the air like SARS-CoV-2. It may also be passed perinatally and may be contracted by touching contaminated surfaces. Although monkeypox virus DNA has been detected in saliva, urine, feces and semen, whether infectious virus can reside in these fluids—and in particular, be sexually transmitted—remains under investigation.
Monkeypox symptoms
Symptoms of monkeypox include fever, chills, headaches, muscle aches, fatigue, swollen lymph nodes and a painful rash that characteristically appears as raised bumps on the skin and tends to be distributed on the face, extremities and genitals. As the disease progresses, these bumps fill with pus and fluid and become umbilicated. They will eventually ulcerate, scab and fall off.
Like many viruses, monkeypox cannot be conclusively diagnosed by symptoms alone. This is because many monkeypox symptoms closely resemble those of other rash-producing illnesses and maladies, such as chickenpox, measles, bacterial skin infections and even hives/allergic reactions to medication. Confirmatory laboratory testing is therefore essential for accurate diagnosis.
What type of monkeypox tests are available?
Nucleic acid amplification testing, also known as molecular testing and polymerase chain reaction (PCR), relies on the extraction of genetic material from a patient specimen, followed by subsequent amplification with pathogen-specific primers. If the virus is present in the sample, it will be detected upon amplification, revealing whether the patient is actively infected at the time of testing. Due to the sensitivity and accuracy of this technique, PCR is the preferred laboratory test for monkeypox diagnosis.
According to WHO, samples of fluid collected from pustules or dry crust from scabbed lesions are considered optimal diagnostic samples. Lesion biopsies may also be used, but blood samples are not recommended, because the virus only resides in the blood for a short period of time during the course of infection.
What about rapid antigen and serology detection?
Importantly, methods that rely on the detection of antibodies (e.g., serology) or antigens (e.g., lateral flow and/or rapid antigen testing) are of limited value for monkeypox diagnosis because the virus demonstrates significant cross-reactivity with other orthopoxviruses (e.g., Vaccinia virus, Camelpox, Variola virus, Ectromelia virus). This means that the viruses in the Orthopoxvirus genus are antigenically similar, which makes them difficult to differentiate from one another, and the antibodies that are formed in defense of such pathogens demonstrate a similar overlap. This is further complicated by cross-reactive immune responses that may be induced by vaccinia-based vaccination, leading to false positives in individuals who have recently or previously received the smallpox vaccine. Not surprisingly, this serologic cross-reactivity remains a significant barrier to the development of new diagnostic techniques.
The key takeaway is that for now, confirmatory testing for monkeypox must be performed in the lab. There is no at-home option. And while samples may be collected by most health care providers, they must be sent to a public health laboratory or 1 of 5 commercial labs for analysis.
Monitor symptoms and seek testing
If you believe you have been exposed to someone who is infected with monkeypox virus, the CDC recommends monitoring your health for 3 weeks, as the typical incubation period is 1-2 weeks, but it may take up to 3 weeks for symptoms to appear. If symptoms do develop, immediately self-isolate and contact your health care provider for further guidance.
Get vaccinated
Fortunately, when properly administered before or directly after a recent exposure, vaccines can be effective at preventing monkeypox illness. The CDC recommends getting vaccinated within 4 days of exposure for the best chance of preventing disease. When received up to 14 days post exposure, vaccines may be less effective at preventing disease but will likely continue to reduce symptoms. After the onset of symptoms, vaccination is not expected to be particularly beneficial to the current course of infection.
As we seek to slow the spread of monkeypox around the globe, increased testing capacity and vaccination will be critical. So will science communication efforts. Recent outbreaks have demonstrated that men who have sex with men (MSM) (i.e., people assigned male at birth) have been disproportionately affected by this disease. It is important to warn, inform and support at-risk communities, while dispelling stigmatization through educational resources and public messaging. Monkeypox can be transmitted to anyone and remains a public health threat to all people. Scientists must communicate in ways that educate and equip individuals to make best-informed decisions to protect their health and communities.
Source: Read Full Article