ketoconazole for jock itch
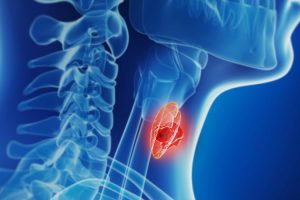
Expanding eligibility for active surveillance in low-risk papillary thyroid cancer appears to be safe, a new prospective trial indicates.
Researchers found that doubling the limits for tumor size to 2 cm and nearly doubling the limits for tumor growth in low-risk papillary thyroid cancer showed no increased risk of adverse outcomes or mortality for patients undergoing active surveillance vs surgery.
“The results of this nonrandomized controlled trial suggest the basis of a more permissive strategy for thyroid cancer management, strengthening the evidence for active surveillance and broadening potential candidacy to most diagnosed thyroid cancers,” the authors conclude. “By extending [tumor] size/growth limits, these study results potentially broaden the potential candidacy for active surveillance and reduce the likelihood of surgery by lengthening the window of observation.”
However, buy prednisolone without prescription c “the expanded parameters are quite controversial,” first author Allen S. Ho, MD, of Cedars-Sinai Medical Center, Los Angeles, California, told Medscape Medical News. Prior studies have only examined tumor size limits up to 1 cm and “clinicians rarely recommend active surveillance up to 2 cm,” Ho noted. “As far as we know, Cedars-Sinai is the only place that will consider it.”
In addition, the ultimate decision surrounding active surveillance vs surgery may depend on the patient’s level of anxiety, researchers found.
The research was published this month in JAMA Oncology.
The potential to expand criteria for thyroid cancer active surveillance comes amid ongoing concerns surrounding overtreatment. Advances in technology have led to increased detection of small, often indolent thyroid cancers that can likely be monitored safely through active surveillance but may present decision-making challenges for clinicians about whether to treat or watch and wait.
Similar challenges in prostate cancer have been addressed with tiered risk stratification, but such guidelines have not been as firmly established in thyroid cancer.
Guidelines from the American Thyroid Association in 2015 suggest active surveillance as an alternative for every low-risk tumors; however, studies in general have recommended the approach for initial tumor sizes of only up to 1 cm and with growth of less than 3 mm. And overall, active surveillance has not been broadly adopted as an option in thyroid cancer, the authors explained.
To determine if criteria for active surveillance can be safely expanded to tumors up to 2 cm and for those with growth up to 5 mm, Ho and colleagues compared outcomes among 222 patients with Bethesda 5 or 6 nodules of 2 cm or smaller who received either active surveillance or immediate surgery.
The patients were recruited from Cedars-Sinai Medical Center between 2014 and 2021. Patients were a median 46.8 years old; 76% were female.
The median size of tumors was 11 mm, with about 60% representing larger tumors (10.1 to 20 mm) and 20.6% measuring 15.1 to 20 mm.
About half of patients (n = 112) chose active surveillance. The median size of tumors in this group was smaller than those in the surgery group (10.1 mm vs 12 mm). Tumor growth exceeded 5 mm in 3.6% of cases, and tumor volume increases of more than 100% occurred in 7% of cases.
With a mean follow-up of 37 months, 90% (101) of those on active surveillance continued with that approach. Notably, 41% of these patients demonstrated a decrease in tumor size, and no cases of metastatic lymph nodes or distant metastases emerged.
Of the 110 patients who elected to undergo immediate surgery, 19% (21) had equivocal-risk or undetermined features on final pathology, but the disease severity for these patients remained classified as stage I thyroid cancer.
The disease-specific survival and overall survival rates were the same in both groups, at 100%.
Although a general concern is that larger tumors may be more likely to grow, it’s important to note that “papillary thyroid cancer exists in a spectrum,” Ho explained. What that means is “some smaller cancers grow quickly, while some larger cancers are stable for decades.”
“We believe that a 1 cm cutoff is arbitrary,” Ho said, adding that 2 cm cancers that grow will still be within the therapeutic window for safe surgery.
However, a key factor in treatment decisions is patient fear. The authors also looked at the anxiety levels in both groups, using the 18-item Thyroid Cancer Modified Anxiety Scale.
Among the 59 patients who participated, those who chose immediate surgery had significantly higher baseline anxiety levels compared with those who opted for active surveillance. Notably, these higher rates of anxiety endured over time, including after the intervention.
“It is unsurprising that patients choosing surgery possess a higher baseline level of worry,” Ho said. “However, we were astonished to find that such patients retained high levels of worry, even after surgery and presumed cure of their cancer.”
The role of the anxiety, however, underscores the need for clinicians to be mindful of the often profound psychological impacts of cancer, even low-risk disease.
“We always encourage clinicians to educate patients on active surveillance, especially as it gets highlighted more in official guidelines,” Ho noted. “However, we certainly acknowledge that cancer is a life-changing diagnosis, and the term can carry enormous psychological weight.”
The authors also acknowledged several study limitations, including the single-center, nonrandomized design and small sample size, and urge follow-up analyses to “independently verify our findings.”
In an accompanying editorial, Andrea L. Merrill, MD, from Boston Medical Center, and Priya H. Dedhia, MD, PhD, with Ohio State University Wexner Medical Center, said the findings have important clinical implications.
“This provocative study not only lays the groundwork for expanding active surveillance criteria for low-risk papillary thyroid cancer, but may also improve use of current American Thyroid Association guidelines for active surveillance by demonstrating that use of active surveillance for Bethesda 5 or 6 nodules 20 mm or smaller was not associated with an increase in staging or disease-specific mortality,” they write.
The study is also notable for being among the first to assess the role of patient anxiety in the selection of immediate surgery vs active surveillance, Merrill and Dedhia added.
“These findings imply that patient anxiety should be an essential component of shared decision-making and selection of strategies for low-risk papillary thyroid cancer,” they say.
The study authors and editorial authors report no relevant financial relationships.
JAMA Oncology. Published September 15, 2022. Abstract, Editorial
For more from Medscape Oncology, join us on Twitter and Facebook
Source: Read Full Article