Detecting the earliest population changes of COVID-19 activity with wearable devices
Today, viral illnesses like COVID-19 are tracked using multiple different methods, including lab data, health care visits and wastewater surveillance. According to new data conducted by scientists at the Scripps Research Translational Institute, this arsenal can be expanded to include wearable technologies like fitness devices and smartwatches—which are showing promise in identifying early population changes in COVID-19 activity.
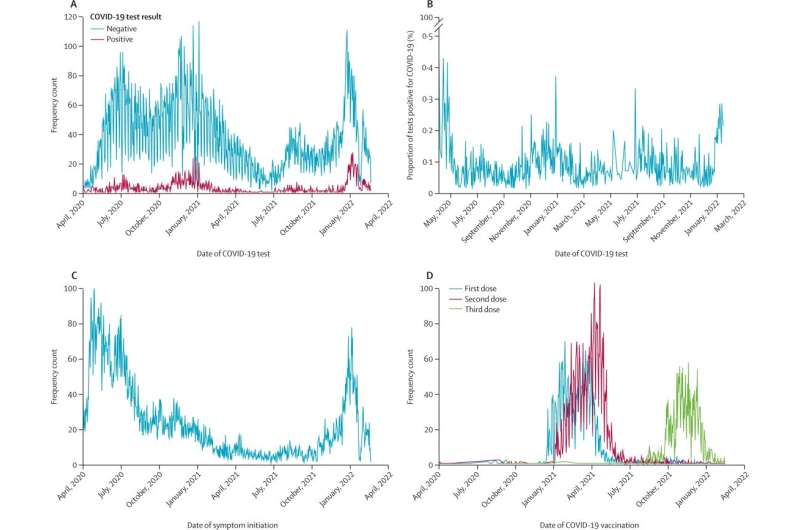
This data comes from the DETECT study: a cross-collaborative effort launched at the onset of the COVID-19 pandemic that uses a mobile app to collect sensor and self-reported information from thousands of study participants across the nation. In addition to the sensor data gathered from a smartwatch, participants can provide details on their test results, vaccinations, symptoms and other demographic information.
In a study published on September 22 in The Lancet Digital Health, the scientists found that sensor data significantly improved the seven-day average predictions for COVID-19 infection. This information can provide an earlier signal than traditional surveillance, as it can identify alterations in a person’s data—potentially even before the participant notices their symptoms. With this promising data in hand, this method of tracking could be expanded to monitor additional infectious disease threats well.
“Wearable technologies give us another valuable piece to the COVID-19 tracking puzzle,” says co-senior author Eric Topol, MD, director and founder of the Scripps Research Translational Institute and executive vice president of Scripps Research. “In aggregating this information at the population level, sensor data provides a unique, real-time picture of how the virus is evolving across the nation.”
Using data gathered from March 25, 2020, to January 14, 2022, the study evaluated factors such as average resting heart rate and step count data across the 39,931 people who participated in the US. Scientists identified a person’s “anomalous” sensor days if they had a higher resting heart rate or lower step count when compared to their baseline data. They then compared these “anomalous” days against a model that predicted the CDC’s seven-day moving averages for COVID-19 cases in real-time, as well as six and 12 days in the future.
In tracking how physiological and behavioral changes may precede symptom onset and eventual testing, the scientists found that this sensor data significantly improved the seven-day average predictions by 32.9% in California—as well as by 12.2% in the United States for predictions occurring 12 days in the future.
The researchers were surprised at how well changes in sensor data tracked with changes in COVID-19 incidence, especially during huge peaks like the Omicron wave.
“All data streams—wastewater, electronic health records, pharmacy information and now sensor data—should be combined if we are to accurately forecast not only COVID-19 transmission, but also viral threats of the future,” says Jennifer Radin, Ph.D., MPH, an epidemiologist at the Scripps Research Translational Institute who is leading the study.
Radin notes that providing a real-time picture for what’s happening in the population is especially relevant now, as more people now test at home rather than in the clinic. And while wastewater surveillance has been a great resource for accomplishing this, the technology can be costly and isn’t available in most of the country.
Source: Read Full Article