Time to Ditch Clarithromycin for H pylori?
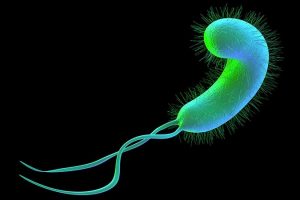
Rates of resistance to clarithromycin among Helicobacter pylori isolates in the United States and Europe are high enough to warrant discontinuation of empiric use of proton pump inhibitor (PPI)–based triple therapy that includes the antibiotic in these regions, a new study has found.
Overall, 22.2% of participants were resistant to clarithromycin — a rate that is above the currently recommended threshold of 15% or higher for avoidance of PPI-based triple therapy that includes clarithromycin.
The results “should put a very big nail in the coffin” of empiric use of such therapies, study investigator William Chey, MD, professor and chief, Division of Gastroenterology and Hepatology, Michigan Medicine, Ann Arbor, told Medscape Medical News.
Judith Kim, MD, a gastroenterologist at NYU Langone Health and clinical instructor of medicine at NYU Grossman School of Medicine in New York City, who wasn’t involved in the study, agrees.
“The use of PPI-based triple therapy is still common practice despite recent recommendations to avoid clarithromycin in areas with high resistance rates,” Kim told Medscape Medical News.
“This study shows that multiple parts of the United States and Europe have high resistance rates,” rendering clarithromycin-based regimens “more likely to ineffectively eradicate H pylori,” Kim said.
The study was published online in The American Journal of Gastroenterology.
Better Options Now Available
Guidelines advise against the use of PPI-based triple regimens with clarithromycin for H pylori infection in areas where resistance is 15% or higher or for patients who have previously received macrolides. However, up-to-date information on H pylori antimicrobial resistance patterns is limited, especially in the United States.
Chey and colleagues assessed resistance rates to antibiotics commonly used to treat H pylori in isolates from 907 adults with the infection in the United States and Europe. They included four US subregions and five participating European countries.
In all US subregions and European countries, clarithromycin resistance rates were above 15% except possibly in the United Kingdom, where the sample size was too small to provide a reliable estimate.
Three quarters of the clarithromycin-resistant isolates were also resistant to metronidazole.
The study also found that, overall, 1.2% of patients had isolates that were resistant to amoxicillin, and 69.2% had isolates resistant to metronidazole. Resistance patterns were similar in the United States and Europe; metronidazole resistance was the most common (50% to 79% of isolates), and amoxicillin was the least common (≤5%).
“Overall, these data provide robust evidence to support a shift away from the default empiric prescription of triple combinations containing a PPI and clarithromycin for H pylori infection in the US and Europe,” the study team writes.
The high prevalence of resistance, including dual resistance, highlights the need for antibiotic stewardship and resistance surveillance, as well as novel treatment strategies for H pylori infection, they add.
Last spring, as previously reported by Medscape Medical News, the US Food and Drug Administration approved two vonoprazan-based treatments for H pylori: Voquezna Triple Pak (vonoprazan, amoxicillin, clarithromycin) and Voquezna Dual Pak (vonoprazan, amoxicillin), both from Phathom Pharmaceuticals.
“Vonoprazan-based treatment may be superior to standard PPI triple therapy for clarithromycin-resistant infections based on prior studies and is a potential good option,” Kim said.
Still, Kim added, she “would most likely first recommend regimens that do not have clarithromycin, such as bismuth quadruple therapy.”
Study’s Importance
Because the study drew upon the largest dataset to date on US resistance rates, it should be used to more precisely guide first-line therapy decisions, said Richard Peek, Jr, MD, professor of medicine and director of gastroenterology at Vanderbilt University Medical Center in Nashville, Tennessee.
“To date, there has been a dearth of information in the United States regarding H pylori resistance rates, which has often led to the use of ineffective empiric therapies and inappropriate exposure to antibiotics,” Peek, who wasn’t involved in the study, told Medscape Medical News.
“These data are particularly exciting when viewed within the context of new genomic sequencing tests that can determine H pylori resistance patterns using DNA isolated from the stomach or the stool,” he said.
Peek agreed that the recent approval of vonoprazan-based therapies “adds another regimen to the therapeutic armamentarium available for eradicating H pylori, and its value seems to be particularly beneficial for eradication failures.”
The research was funded by Phathom Pharmaceuticals. Chey is a board member of the American College of Gastroenterology, GI on Demand, the International Foundation of Functional GI Disorders, and the Rome Foundation. He has received compensation as a consultant from AbbVie, Alfasigma, Allakos, Alnylam, Bayer, BioAmerica, Cosmo, Intrinsic Medicine, Ironwood Pharmaceuticals, QOL Medical, Nestle, Phathom Pharmaceuticals, RedHill Biopharma, Salix/Valeant, Takeda, Urovant, and Vibrant; grant/research support from BioAmerica, Commonwealth Diagnostics International, QOL Medical, Salix, and Vibrant; owns stock/stock options in GI on Demand and Modify Health; and owns patents relating to methods and kits for identifying food sensitivities and intolerances, digital manometry, and a rectal expulsion device. Peek and Kim report no relevant financial relationships.
Am J Gastroenterol. Published online September 30, 2022. Abstract
For more news, follow Medscape on Facebook, Twitter, Instagram, and YouTube.
Source: Read Full Article