Escorting a key immune protein to its demise to control inflammation
Monash University researchers have discovered a key mechanism in the body’s immune system that helps control the inflammatory response to infection. The discovery could help pave the way for more targeted therapies in a range of inflammatory conditions, such as autoimmunity and neuroinflammatory disease.
The innate immune system is the body’s first line of defense against pathogens. Innate immune proteins detect foreign bodies such as bacteria and viruses and respond by mounting a protective inflammatory immune response to destroy the invading pathogen.
A tightly regulated inflammatory response that is precisely turned on and then off is key for host protection against infection. However, in some instances these pathways can be unnecessarily switched on and not off, effectively leading to autoimmune and neurodegenerative diseases.
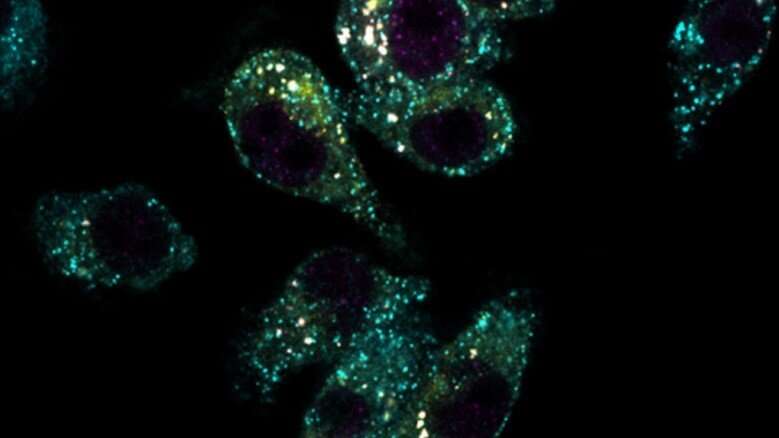
Research published in The EMBO Journal studied the complex chain of events involved in the inflammatory response that is mediated by a key innate immune protein Stimulator of Interferon Genes (STING).
Monash Biomedicine Discovery Institute’s (BDI) Senior Researcher Dr. Dominic De Nardo explained the significance of the findings.
“The innate immune system is ancient in our evolutionary history and is very robust,” Dr. De Nardo said.
“The different components within the system are involved in detecting pathogens, mounting an inflammatory immune response, which should ultimately aid in the clearance of the threat, then signaling to the system that it’s time to shut off the inflammation.”
“My group focuses on inflammatory responses induced by a central innate immune receptor—called Stimulator of Interferon Genes, or STING—that can alert the body to danger from pathogens, or be turned on by factors from within our own body that appear in the wrong place.”
“The goal is to slow down and stop damaging inflammation in disease, driven by unwarranted turning on and/or inefficient shutting off of STING. We are looking forward to advancing this research further into human immune cells and pre-clinical studies.” First author and recently graduated Ph.D. student, Dr. Kate Balka, said the team wanted to understand how STING immune responses were regulated to ensure effective host immunity.
“We know on the one hand that STING responses are crucial for clearing pathogens, but on the other, unrestrained STING activity causes several inflammatory diseases including autoinflammatory, autoimmune and neurodegenerative conditions,” Dr. Balka said.
“In other words, we wanted to understand and answer the question, how is STING turned off?”
The researchers determined the precise mechanisms controlling the termination of STING responses.
“In this study we have determined the molecular machinery, known as endosomal sorting complex required for transport (ESCRT), that packages STING into small compartments to allow it to be degraded, or broken down, by the lysosome—the cell’s ‘trash compactor’,” Dr. De Nardo said.
By understanding this critical step of STING regulation, new avenues for potential therapeutic targeting of STING in disease pathologies can be pursued.
More information:
Katherine R Balka et al, Termination of STING responses is mediated via ESCRT ‐dependent degradation, The EMBO Journal (2023). DOI: 10.15252/embj.2022112712
Journal information:
EMBO Journal
Source: Read Full Article