synthesis of prednisone

Artificial intelligence (AI) techniques may provide a more accurate approach to predicting the risk of periprosthetic infection after implant-based breast reconstruction, reports a study in the November issue of Plastic and Reconstructive Surgery
“Our study shows promise in using artificial intelligence and machine learning to improve the ability to predict the risk of serious postoperative complications in patients undergoing breast reconstruction after mastectomy,” comment ASPS Member Surgeon, senior and corresponding author Charles E. Butler, the pharmacy drug zithromax MD, and first author Abbas M. Hassan, MD.
AI lends insights into complex risk factors for periprosthetic infection
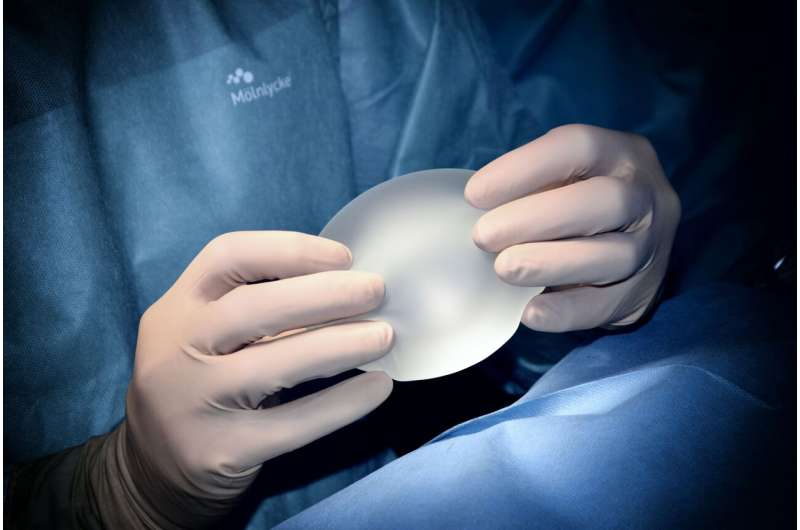
Periprosthetic infection—infection developing around an implant—is a common and serious complication of implant-based breast reconstruction after mastectomy. Although tools have been developed to provide individualized assessments of the risks associated with breast reconstruction, conventional statistical techniques may fail to analyze the “complex nonlinear interactions” affecting the risk of complications.
Dr. Butler and colleagues evaluated the use of machine learning, to evaluate variables that place patients at higher or lower risk of implant-related complications, including infection and explantation. The researchers developed, validated, and evaluated the use of nine supervised machine learning algorithms to predict the risks of periprosthetic infection and explantation (implant removal). Data on a random sample of 80% of patients were served as a training set and the remaining 20% as a testing or validation set.
The AI approach was developed using data on a total of 694 implant-based breast reconstructions in 481 patients, average age 50 years. Over a median follow-up of 16 months, periprosthetic infection developed in 16.3% of reconstructions, with an explantation rate of 11.8%.
Machine learning algorithms increase accuracy in predicting complication risks
For periprosthetic infection, predictive accuracy ranged from 67% to 83%, with a “random forest” algorithm being most accurate. This model identified nine predictive factors; the strongest predictors were higher body mass index (BMI), older age, and postoperative radiation therapy.
For explantation, accuracy ranged from 64% to 84%, highest with an “extreme gradient boosting” algorithm. This approach identified 12 significant predictors, including patient characteristics (higher BMI, older age), surgical characteristics (implant location and use of certain biomaterials), and cancer treatment variables (postoperative radiation or chemotherapy).
For both outcomes, the machine learning algorithms performed better than a standard statistical model—the Breast Reconstruction Risk Assessment or “BRA score”—in predicting both infection and explantation. The area under the curve (AUC), ranging from 0.5 to 1.0, determines the overall performance of predictive models and values of 1.0 signify “perfect discrimination” while a value of 0.5 means no predictive value. Prediction of infection with machine learning models showed an AUC of 0.73, and 0.78 for explantation, compared to under 0.60 in previous studies using the BRA score.
A key advantage of the machine learning algorithms is that they identified more predictive variables: nine predictors of infection and 12 of explantation, compared to just two for standard statistical (multivariable) analysis. “This provides broader and more robust understanding of factors that negatively impact outcomes in patients who undergo breast reconstruction and can help guide future research to better understand disease processes and provide accurate risk prediction for patients with multiple comorbidities,” say Drs. Butler and Hassan.
The researchers emphasize that risk prediction with machine learning remains “far from perfect”—but “may be improved by incorporating additional clinically relevant variables.” Dr. Butler and co-authors conclude: “AI has the potential to reshape the field of plastic surgery and improve the quality of care for cancer patients by more precisely and accurately identifying factors that lead to poor outcomes.”
More information:
Abbas M. Hassan et al, Artificial Intelligence Modeling to Predict Periprosthetic Infection and Explantation following Implant-Based Reconstruction, Plastic & Reconstructive Surgery (2023). DOI: 10.1097/PRS.0000000000010345
Journal information:
Plastic and Reconstructive Surgery
Source: Read Full Article