How depressed T cells contribute to chronic immune diseases

In chronic infections, the immune system can become exhausted. Ludwig-Maximilians-Universitaet (LMU) in Munich researchers have looked into how this works.
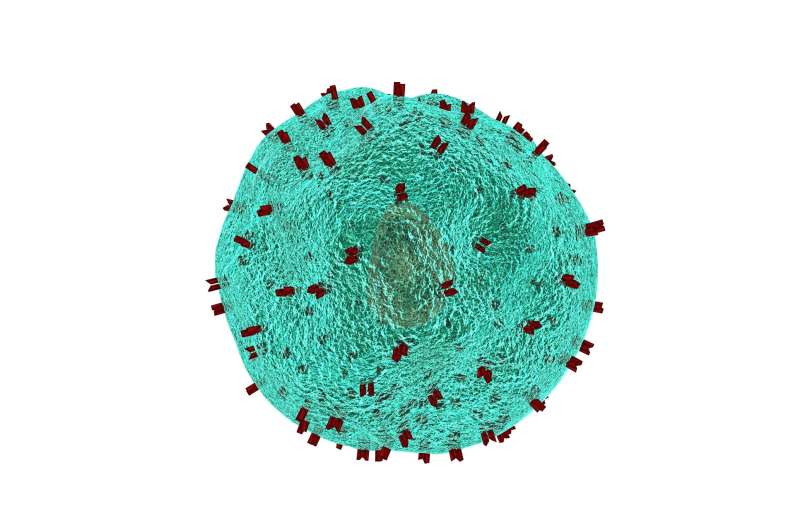
T lymphocytes, or T cells, are an important component of our immune system. They can recognize foreign proteins, so-called antigens, as peptide fragments—for instance, those derived from viruses or cancer cells. In principle, they could, but usually do not, attack our own (“self”) proteins. “That is why it is important for the organism to tightly control the activities of T cells,” says Dr. Reinhard Obst, head of a research group at the Institute for Immunology at LMU’s Biomedical Center that studies the activation of T cells.
When viruses gain access to tissues, T cells are activated to eliminate the pathogens. However, if T cells are exposed to their target antigens for too long, they can lose their functionality and become “exhausted.” They no longer secrete pro-inflammatory messenger molecules, and therefore cannot contribute much to an immune response. On the one hand, it makes sense to keep these cells under control so as to avoid collateral damage to the organism. On the other, T cell exhaustion makes it difficult to fight chronic diseases, such as those caused by HIV, hepatitis viruses and cancer cells. Understanding immune responses to chronically persisting threats like these is thus one of modern medicine’s great challenges. “This is where T cell exhaustion plays a central role.” the LMU researcher says.
A new model to study T cell exhaustion
Several years ago, Obst developed an animal model which has now yielded important insights. He focused on T helper cells, which express the CD4 marker molecule and make up the largest subset of T cells. Each of these cells recognizes a defined protein fragment as an antigen.
To control the timing and the amount of the specific antigen expressed in this model system, the LMU scientists used a trick. Their transgenic mice were exposed to different doses of the antibiotic doxycycline, which controls the synthesis of the antigen, via their drinking water. Different amounts of antigen are thus being presented to the T cells in these animals, which avoids the need for experimental infection. “In this way, we are able to regulate the amount of antigen produced,” Obst explains. “Our goal was to find out how the corresponding T helper cells respond.
The results showed that the effects were dose dependent: In the presence of high antigen doses, the T cells underwent apoptosis, meaning they died by programmed cell death. At an intermediate dose, however, the T cells survived but quickly lost their functionality. “We demonstrated this state of exhaustion by regulating the amount of antigen that the cells encountered,” the LMU researcher explains. At a low dose, it took several weeks before the cells showed signs of exhaustion. When in further experiments the antigen was subsequently removed, the cells were able to partially recover from their exhausted state. Such dynamic adjustments convinced the researchers that T-helper cells are capable of a surprising degree of plasticity.
Supporting the T cells’ fight against chronic infections and cancer
Obst and his colleagues believe that their findings could have therapeutic implications. The data indicate that a number of transcription factors (proteins that control gene expression) and signaling pathways regulate the different states of exhaustion.
Two years ago, several groups showed that one of these transcription factors, named Tox, contributes significantly to the exhaustion of T killer cells, another T cell subset. When the Tox gene was deleted, the T-killer cells were less readily exhausted in a chronic infection and could more effectively fight a chronically persisting virus. However, they also attacked the host animals’ organs and died sooner. The new findings suggest that there are several mechanisms in place to adjust T helper cells dynamically to different antigen loads.
Source: Read Full Article