COVID pandemic may have driven a flu strain into extinction

It’s well-known that COVID-19 pandemic restrictions pretty much quashed the 2020-2021 flu season, with influenza cases falling to never-before-seen lows in the United States.
So little flu circulated, in fact, that some scientists now suspect that one of the major strains of influenza might have gone extinct, for lack of humans to infect.
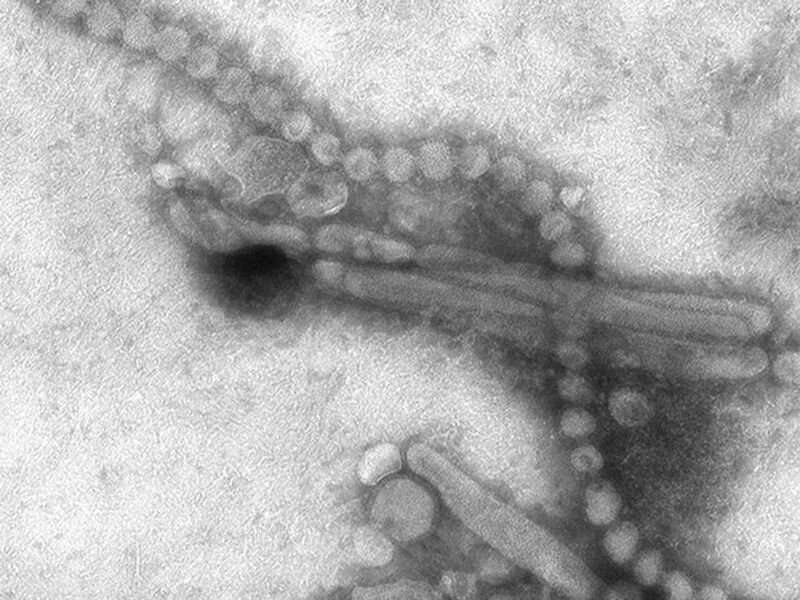
Influenza B/Yamagata is one of four strains regularly included in annual flu shots, but in the midst of COVID lockdowns that strain appears to have fallen completely off the radar, an Australian research team recently reported in the journal Nature Reviews.
No B/Yamagata strains have been isolated or genetically sequenced in flu case tracking since March 2020, when COVID lockdowns essentially ended the 2019-2020 flu season, the researchers said.
Only 31 suspected B/Yamagata cases have been reported to public health officials from the most recent flu season, but there was no successful isolation or sequencing of the virus to determine that B/Yamagata was truly to blame.
B/Yamagata has always tended to be less infectious than the other major flu strains, researchers noted. That strain also doesn’t evolve as energetically as the others; vaccine manufacturers haven’t had to update the B/Yamagata component of the annual flu shot since 2015.
Those factors, “combined with suppressive conditions of the COVID-19 pandemic, may have facilitated strong suppression of global B/Yamagata circulation and the potential extinction of this lineage,” the researchers concluded in their report. Marios Koutsakos, a postdoctoral research fellow at the University of Melbourne, led the study.
If an entire strain of influenza has indeed gone extinct, that would open up new possibilities for tackling the annual flu going forward, American infectious disease experts said.
But they first caution that it’ll take longer than one flu season to determine whether B/Yamagata has bitten the dust.
“I’d be a little leery of calling it a done deal, because flu’s a fickle little beast,” said Richard Kennedy, a top vaccine researcher with the Mayo Clinic in Rochester, Minn.
He noted that B/Yamagata tends to surge in certain years and then virtually disappear in others.
“Just the evidence we haven’t seen it for a while, I don’t think that by itself is a convincing argument,” Kennedy said. “Data suggesting that since we haven’t seen a single case since March 2020, that’s good, but I’d like to see a longer period where we don’t see any of it, because it’s hidden from us before, these lineages.”
Now, COVID restrictions have relaxed and kids are back in school, raising concerns among public health officials that this flu season could be a tough one. B/Yamagata could resurface, he said.
“These viruses are very good at making up for lost time and lost distance in this race,” Kennedy said. “We might get ahead, but if we don’t continue, we can’t get a handle on it.”
If B/Yamagata is truly gone for good, that means we could juggle the strains included in the annual flu vaccine to get more bang for our buck, said Dr. William Schaffner, medical director of the Bethesda, Md.-based National Foundation for Infectious Diseases.
The structure of the current flu vaccine includes four strains: influenza A/H3N2 (Hong Kong), influenza A/H1N1 (Swine), influenza B/Victoria, and influenza B/Yamagata. The influenza A strains tend to be more infectious and the source of deadly epidemics, while influenza B percolates more slowly among school-age children and teens.
Each year U.S. scientists play a guessing game to determine which genetic version of each of the four strains is likely to be the most infectious, Kennedy said. When they guess right, the flu vaccine provides better protection.
Replacing the B/Yamagata part of the vaccine with another strain that’s more infectious and dangerous could improve the shot’s effectiveness, Schaffner said.
“Could you double up on the next most severe strain, H3N2? Could you get two H3N2s in there?” Schaffner said.
Kennedy agreed. “Being able to pick another strain that’s not B, that’s an A strain, would probably help with that guessing game,” he said.
On the other hand, the vaccine could be cut back to just three strains, which would make the shot cheaper and easier to manufacture, Kennedy said.
“You’re able to manufacture more doses or maybe drop the cost a little bit. That makes the vaccine more accessible for everyone,” he said.
If people get the flu shot this year and stick to COVID protections like masking and social distancing, there’s a chance that B/Yamagata might be gone for good, Kennedy and Schaffner agreed.
“We did learn from the last season that if you were profound in your mask wearing and social distancing, staying home, closing schools, limiting travel, you could really profoundly abort the annual influenza outbreak,” Schaffner said. “Some of that I think will come back, and I think we’ll see more of that in conventional public health recommendations.”
As flu enters communities, there will be reminders for folks who are more apt to get more severe disease to put on masks again, he said.
Source: Read Full Article