Cutting-edge molecular tools reveal potential COVID-19 diagnostic and therapeutic targets

Using some of the most advanced molecular sequencing tools available to evaluate COVID-19 rapid autopsy tissues, researchers have identified four major regulatory pathways, specific molecular effectors behind COVID-19 symptoms, and differences that drive diverging clinical courses among individual patients. This research may pave the way for a more personalized and effective approach to COVID-19 diagnosis and treatment, researchers explain in a new study published in The American Journal of Pathology.
“From the time that COVID-19 first hit New York City in March 2020, the Department of Pathology at Mount Sinai made a commitment to uncompromisingly perform as many autopsies as was needed to better understand what causes this complex and devastating illness,” explained lead investigator Carlos Cordon-Cardo, MD, Ph.D., Professor and Chairman, Department of Pathology, Molecular and Cell-Based Medicine, Icahn School of Medicine at Mount Sinai Hospital, New York, NY, USA. “It was clear to us that beyond the very valuable study of these tissues under the microscope, we would need to dissect the molecular pathways that drive the disease and underlie the diverse clinical complications seen in our patients.”
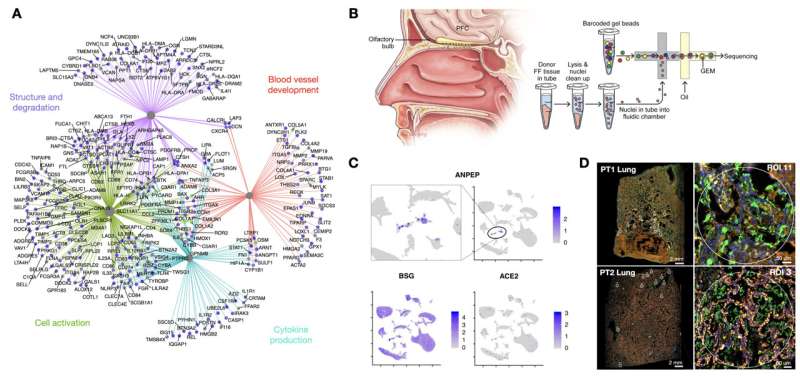
Rapid autopsies were performed on tissues from two decedents with different symptomology using multi-scale RNA next-generation sequencing methods to provide unprecedented molecular resolution of COVID-19–induced damage. Assessing cells individually and integrating histology and molecular information enabled researchers to capture the unique features of each patient’s illness.
Patient 1 was a male in his 60s with a complex medical history whose hospitalization lasted for over a month. Patient 2, also a male in his 60s, had diabetes and heart failure who died shortly after admission.
Bulk RNA sequencing evaluation in Patient 1 revealed viral RNA in the nasopharynx and lung, but not in the olfactory bulb, prefrontal cortex, oropharynx, salivary gland, heart, liver, or kidney. Comparison of the infected and uninfected tissues revealed four major regulatory pathways. Effectors within these pathways could constitute novel therapeutic targets, such as the complement receptor C3AR1, which can be involved in the development of hyperinflammatory and hypercoagulable states, and decorin, which plays an important role in the extracellular matrix and could affect the regulation of signaling, autophagy, and macrophage activation and fibrosis in response to chronic injury. These are all critical aspects of severe COVID-19 disease and potentially long-term COVID as well.
Single-nuclei RNA sequencing of olfactory bulb and prefrontal cortex in Patient 1 highlighted greater diversity of coronavirus receptors than is routinely evaluated. Examination of multiple coronavirus-associated receptors revealed only scattered expression of angiotensin converting enzyme 2 (ACE2) in rare cells and robust expression of basigin (BSG) throughout. Though significant attention has been paid to the role of ACE2, these results provide evidence of infection potential in the brain via alternative receptors.
Finally, digital spatial profiling was performed on lung and lymph node tissues from both patients, comparing patients with different characteristics and disease courses. The results showed distinct molecular phenotypes that may be related to early- versus late-stage COVID-19.
The researchers note that the potential diagnostic and prognostic markers and therapeutic targets revealed in this study could not have been uncovered through other methods. Current COVID-19 therapies are generally focused on either the virus itself, with antiviral medications and hyperimmune sera, or nonspecific approaches to the inflammatory and coagulopathic challenges, such as steroids and blood thinners.
“In order to develop new classes of therapeutics that can synergize with existing treatments and act on the key effectors driving these symptoms, it is critical to gain a more detailed, molecular understanding of the pathophysiology of severe COVID-19,” concluded lead author Elisabet Pujadas, MD, Ph.D., also of the Department of Pathology, Molecular and Cell-Based Medicine, Icahn School of Medicine at Mount Sinai, New York, NY, USA.
Source: Read Full Article