Drug deaths in England and Wales rise for eighth consecutive year


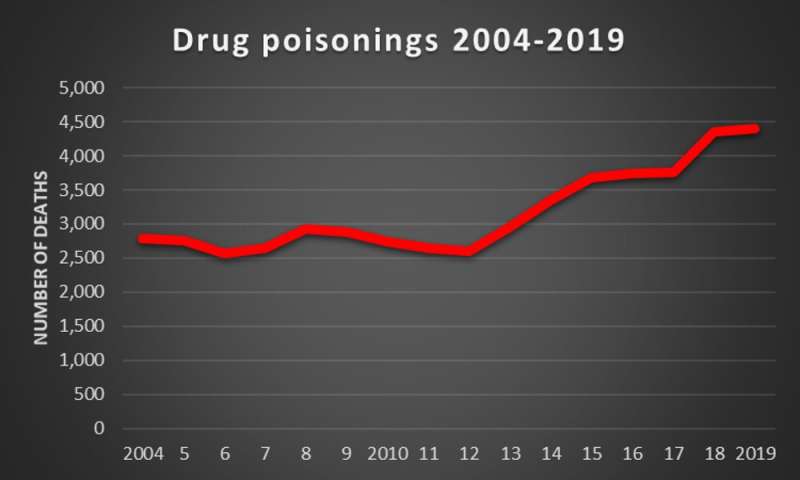
Coronavirus is a public health crisis for all of society, but for the past decade, people who use drugs—especially those dependent on opioids—have been facing their own epidemic. In its annual report on drug poisoning in England and Wales, the Office for National Statistics (ONS) reveals that 4,393 died in 2019—yet another rise from 2018.
This is the highest number of drug-related deaths since records began, and the north-east of England has a significantly higher rate than other English regions—another trend that has continued. The most deprived communities have rates of deaths that are five-and-a-half times greater than the least deprived.
Although drugs such as heroin still account for most of these deaths, this year sees a significant jump in deaths due to cocaine use. Male deaths attributed to cocaine rose 7.7% while female deaths rose by 26.5%. Men are known to take greater risks with drugs than women, so it is difficult to understand why there is such a marked difference between the sexes.
As with COVID, counting these deaths is far from perfect. Pinpointing the exact cause of death and then ensuring this is recorded and reported in a timely way can be difficult.
Decade of austerity
There is a significant time lag between a death occurring and it appearing in official data. What we can say with certainty is that these tragic and avoidable deaths, like those resulting from the coronavirus, are more likely to occur in communities living in deprivation. What these dual public health crises have shown is that structural inequalities are fuelling death. Leaving these communities paying for failed government policies and serious disinvestment in public services caused by a decade of austerity.
As the COVID pandemic has evolved, the government is happy to ignore its own expert advice, and block critical voices on drug policy. The Advisory Council on the Misuse of Drugs, the UK government’s own expert drug advisers, recommended protecting and increasing investment in drug treatment and that consideration be given establishing drug-consumption rooms. Dame Carol Black, who was commissioned by the government to review the harm caused by drugs, found that there had been a 17% cut to treatment budgets since 2014-15.
Kit Malthouse, the UK’s minister for drugs, referred to drug-consumption rooms as a “distraction” at the UK Drugs Summit held in Glasgow in February 2020, again ignoring the advice of the government’s own experts. This left it to a member of the public in Glasgow to set up a drug consumption van in the city, despite a risk of prosecution.
Beyond the tragic deaths reported today, Dame Carol Black found that while 2,889 people in contact with specialist drug-treatment centers died in 2018-19, this rose to nearer 5,000 when other factors were included. The lower figure relates to those who have died from a fatal overdose, for example, but people who use drugs are at greater risk of liver disease or respiratory problems because of their lifestyles, which can also be fatal. Again, structural inequalities, lack of investment in treatment and the politicization of evidence-based interventions have all contributed to this public health crisis.
There is some hope, COVID has, out of necessity, prompted an improved digital treatment offering. This provides everything from video conferencing and virtual therapeutic groups to individual phone calls from therapists. Unfortunately, some patients don’t have access to this technology, but it could nevertheless go some way to improving engagement and retention in treatment for some. And being in treatment is associated with a reduced risk of fatal overdose.
The downside is that digital-based services are only available to those with the ability to access and understand them. Equally, some may miss the human contact that therapists and therapeutic groups provide. A blend of both digital and face-to-face would provide an optimum offering.
Less restrictive prescribing practices, which have seen people moved off daily supervised consumption of their medication onto seven or 14-day prescriptions, has also yielded positive results. This is important, as opiate substitute medications have been shown to be the only treatment interventions that can prevent fatal overdoses.
From denial to acceptance
There is much we can learn from the COVID-19 crisis about reducing harm from drugs, not least that policy needs to be timely and not hindered by political dogma. The time for talking about reform of drug policy has passed, increasing numbers are dying due to this paralysis in policy.
Source: Read Full Article