Engineering an ‘invisible cloak’ for bacteria to deliver drugs to tumors


Columbia Engineering researchers report that they have developed a “cloaking” system that temporarily hides therapeutic bacteria from immune systems, enabling them to more effectively deliver drugs to tumors and kill cancer cells in mice. By manipulating the microbes’ DNA, they programmed gene circuits that control the bacteria surface, building a molecular “cloak” that encapsulates the bacteria.
“What’s really exciting about this work is that we are able to dynamically control the system,” said Tal Danino, associate professor of biomedical engineering, who co-led the study in collaboration with Kam Leong, Samuel H. Sheng Professor of Biomedical Engineering. “We can regulate the time that bacteria survive in human blood, and increase the maximum tolerable dose of bacteria. We also showed our system opens up a new bacteria delivery strategy in which we can inject bacteria to one accessible tumor, and have them controllably migrate to distal tumors such as metastases, cancer cells that spread to other parts of the body.”
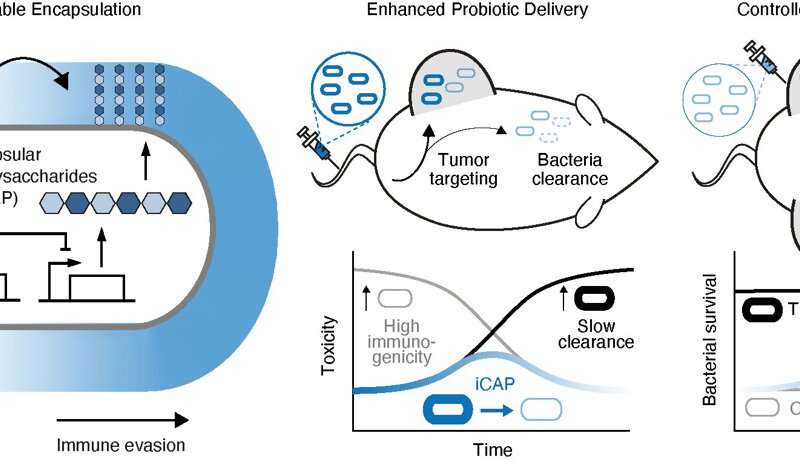
For the study published today by Nature Biotechnology, the researchers focused on capsular polysaccharides (CAP), sugar polymers that coat bacterial surfaces. In nature, CAP helps many bacteria to protect themselves from attacks including immune systems. “We hijacked the CAP system of a probiotic E. coli strain Nissle 1917,” said Tetsuhiro Harimoto, a Ph.D. student in Danino’s lab who is the study’s co-lead author. “With CAP, these bacteria can temporarily evade immune attack; without CAP, they lose their encapsulation protection and can be cleared out in the body. So we decided to try to build an effective on/off switch.”
An effective on/off switch
To do this, the researchers engineered a new CAP system, which they call inducible CAP, or iCAP. They control the iCAP system by giving it an external cue—a small molecule called IPTG—that allows for programmable and dynamic alteration of the E. coli cell surface. Because iCAP alters bacterial interactions with immune systems (such as blood clearance and phagocytosis) in a directed manner, the team found that they could control the time to which bacteria can survive in human blood, by tuning how much IPTG they give to the iCAP E. coli.
Using bacteria for therapy
While using bacteria for therapy is a new, alternative approach to treating a broad array of cancers, there are a number of challenges, in particular, their toxicity. Unlike many traditional drugs, these bacteria are alive and can proliferate within the body. They are also detected by the body’s immune systems as foreign and dangerous, causing high inflammatory response—too much bacteria means high toxicity due to over-inflammation—or rapid bacteria elimination—too little bacteria means no therapeutic efficacy.
Jaeseung Hahn, a postdoctoral research scientist in Danino and Leong’s labs who co-led the project, noted, “In clinical trials, these toxicities have been shown to be the critical problem, limiting the amount we can dose bacteria and compromising efficacy. Some trials had to be terminated due to severe toxicity.”
The ideal bacteria
The ideal bacteria should be able to evade the immune system upon entry to the body, and efficiently get to the tumor. And once they are in the tumor, they need to be eliminated in other parts of the body to minimize toxicity. The team used mouse tumor models to demonstrate that, through iCAP, they could increase the maximum tolerable dose of bacteria 10 times. They encapsulated the E. coli strain to enable it to evade the immune system and get to the tumor. Because they did not give IPTG in the body, the E. coli iCAP lost its encapsulation over time, and was easier to be eliminated in other parts of the body, thus minimizing toxicity.
To test efficacy, the researchers then engineered E. coli iCAP to produce an antitumor toxin and were able to shrink tumor growth in colorectal and breast cancer mouse models more so than in the control group without the iCAP system.
The team also demonstrated controllable bacterial migration within the body. Past studies have shown that low levels of bacteria leak out from tumors upon tumor growth. For this new study, the Columbia team used iCAP to show that they can control bacterial leakage from a tumor, as well as their translocation to other tumors. They injected E. coli iCAP into one tumor, fed the mice with water containing IPTG, activated iCAP within a tumor, and saw E. coli iCAP leak out and migrate to uninjected tumors.
Next steps
The group is exploring a range of research areas. There are more than 80 different types of CAP that exist just for E. coli and even more for other bacteria species that could be engineered using similar approaches. In addition, CAP is not the only molecule that bacteria have on their surface, and other surface molecules could be controlled in a similar fashion. Additionally, while iCAP is controlled by an externally provided IPTG in this example, other control systems such as biosensors could be used to autonomously control surface properties of therapeutic bacteria.
The team, also affiliated with Columbia’s Herbert Irving Comprehensive Cancer Center and Data Science Institute, notes that clinical translation is the next major challenge they would like to tackle. “While there is a good deal of laboratory research showing various ways to engineer microbes, it is very difficult to apply these powerful therapies to a complex animal or human body. We’ve shown proof of concept in mouse models, but given that humans are 250 times more sensitive to bacterial endotoxins than mice, we expect our results may have an even bigger effect on human patients than on mice,” said Harimoto.
Source: Read Full Article