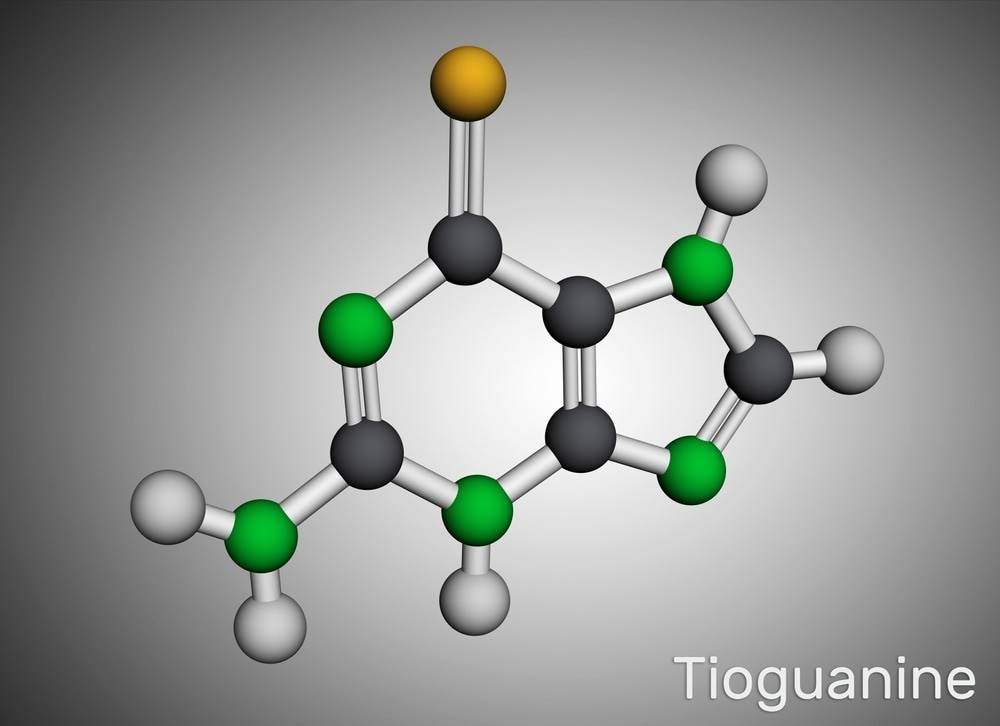
New antiviral mechanism of action for an FDA-approved thiopurine known as 6-thioguanine

In a recent study published in PLoS Pathogens, researchers described a novel antiviral mechanism of action for an FDA (food and drug administration)-approved thiopurine known as 6-thioguanine (6-TG).
Background
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic has spurred efforts to repurpose drugs to develop effective and safe antivirals. Host-targeted antivirals (HTAs) indirectly inhibit viral replication by inhibiting host cellular processes and/or stimulating antiviral responses.
The authors of the present study previously demonstrated that thiopurines, 6-thioguanosine (6-TGo) and 6-TG inhibit IAV (influenza A virus) replication by unfolded protein response (UPR) activation and interfering with the viral glycoprotein processing and accumulation.
About the study
The present study investigated whether 6-TG and other thiopurines could interfere with coronavirus (CoV) glycoproteins.
Thiopurine efficacy against severe SARS-CoV-2, human CoV (HCoV)-OC43 and HCoV-229E replication inhibition and disruption of viral ribonucleic acid (RNA) synthesis were assessed. Cell culture experiments were performed using 293T cells, HCT-8 (human ileocecal adenocarcinoma cell line), Huh7.5 (human hepatoma-derived cell line), primary human telomerase reverse transcriptase (hTERT)-immortalized fibroblast and Calu-3 (lung adenocarcinoma cell line) cells.
Further, viral particle release was assessed by quantitative reverse transcription-polymerase chain reaction (RT-qPCR) analysis of extracellular viral genomes. Immunostaining analysis using HCoV-OC43-infected cells was performed for anti-nucleocapsid (N) antibodies and double-stranded RNA (dsRNA). Ribopuromycinylation assays were performed, and 293T cells were transfected with plasmids encoding SARS-CoV-2 structural proteins such as N, spike (S), membrane (M), and envelope (E) proteins to evaluate the impact of 6-TG on SARS-CoV-2 structural proteins.
Further, SARS-CoV-2 S was ectopically expressed and assessed against multiple 6-TG concentrations, following which immunoblotting analysis with pseudovirions (PV) was performed. S-expressing 293T cell lysates were treated with PNGase F (peptide-N-glycosidase) to eliminate N-linked glycans from polypeptide chains, and the effects of 6-TG on the secretory pathway were assessed by Gaussia luciferase assays.
Flow cytometry (FC) analysis and surface staining of S-expressing 293T cells were performed to measure S secretion, and the cells were co-transfected with EGFP+ (enhanced green fluorescent protein) plasmids to assess alterations in S protein accumulation.
Furthermore, cell co-transfections with SARS-CoV-2 structural proteins and plasmids were performed to elucidate the defective assembly mechanisms, and the team determined if any known 6-TG targets cause S protein maturation defects. The team also assessed potential HCoV morphological alterations after 6-TG treatment by transmission electron microscopy (TEM) analysis.
Results
Genetics & Genomics eBook

Compilation of the top interviews, articles, and news in the last year.
Download a copy today
6-TG inhibited the initial stage of SARS-CoV-2 and HCoV-OC43 replication, limiting full-length viral genome, structural proteins and subgenomic RNA accumulation. Ectopic S expression analysis showed enhanced S protein electrophoretic mobility from several βCoVs by 6-TG treatment, in accordance with the in vitro enzymatic N-linked oligosaccharide elimination from the S protein. SARS-CoV-2 VLPs (virus-like particles) in 6-TG-treated cells lacked the S protein.
Similar 6-TG effects were observed on SARS-CoV-2 S-pseudotyped lentivirus production yielding S-deficient pseudoviruses that could not infect angiotensin-converting enzyme 2 (ACE2)-expressing cells. The findings indicated that 6-TG treatment led to defective S protein processing and trafficking and thereby impeding infectious progeny virus assembly. However, the conversion of 6-TG to its nucleotide (nt) form by HPRT1 (hypoxanthine phosphoribosyltransferase 1) was essential for antiviral activity, which could be overcome by ML099, a guanosine-5'-triphosphate (GTP)ase agonist.
No GTPase inhibitors [Ras-related C3 botulinum toxin substrate 1 (Rac1), Ras homolog family member A (RhoA), and Cell division control protein 42 homolog (CDC42)] affected S accumulation or processing, indicating that 6-TG inhibited S maturation by inhibiting an unknown cellular GTPase. 6-TG, 6-thioguanosine (6-TGo), and 6-mercaptopurine (6-MP) caused four-log reductions in SARS-CoV-2 virion release and 6-TGo showed comparable HCoV-OC43 and HCoV-229E inhibition, whereas 6-MP was ineffective. The RT-qPCR analysis showed that 6-TG treatment reduced HCOV-OC43 titers by 20-fold on the initial day of infection.
Putative full-length genomic viral RNA was reduced by 10-fold in most stages of infection. 6-TG treatment caused similar reductions in viral S- and N-encoding sub-genomic RNA correlating with lower protein accumulation. Immunostaining HCoV-OC43-infected cells with anti-N antibodies showed punctate staining initially and peripheral staining subsequently. Post-6-TG treatment, the stained areas were brighter, with large puncta observed after 24 hours post-infection (hpi). Immunostaining for dsRNA showed considerably reduced dsRNA signals among 6-TG-treated cells.
6-TG delayed or suppressed UPR downstream transcriptional responses but did not affect the translation initiation rates in HCoV-OC43-infected cells. 6-TG inhibition of HCoV-OC43 infection restricted inositol-requiring enzyme 1 (IRE1) activation and X-box binding protein 1 (XBP1s) target gene accumulation. The findings indicated that even though 6-TG interfered with viral full-length genomic and subgenomic RNA synthesis, host shutoff was unperturbed.
6-TG reduced SARS-CoV-2 structural protein (especially S) expression and immunoblotting analysis showed a high molecular weight S-band denotive of the S0 precursor protein, which was also sensitive to PNGaseF treatment. The electrophoretic mobility analysis findings indicated that 6-TG inhibited S glycosylation and processing, and Gaussia luciferase experiments showed that 6-TG didn’t cause global secretory pathway disruption. The TEM analysis showed fewer viral particles in 6-TG-treated cells.
Conclusion
Overall, the study findings highlighted small GTPases as potential HTA targets, and the effects of 6-TG on S in several models, such as ectopic expression, authentic HCoV infections, and production of PVs and VLPs, indicate an antiviral mechanism beyond papain-like protease (PLpro) inhibition.
- Pringle, E. et al. (2022) "Thiopurines inhibit coronavirus Spike protein processing and incorporation into progeny virions", PLOS Pathogens, 18(9), p. e1010832. doi: 10.1371/journal.ppat.1010832. https://journals.plos.org/plospathogens/article?id=10.1371/journal.ppat.1010832
Posted in: Medical Science News | Medical Research News | Disease/Infection News
Tags: ACE2, Adenocarcinoma, Agonist, Angiotensin, Angiotensin-Converting Enzyme 2, Antibodies, Cell, Cell Culture, Cell Division, Cell Line, Coronavirus, Cytometry, Drugs, Efficacy, Electron, Electron Microscopy, Enzyme, Fibroblast, Flow Cytometry, Fluorescent Protein, Food, Gene, Genome, Genomic, Glycans, Glycoprotein, Glycosylation, in vitro, Influenza, Inositol, Lentivirus, Luciferase, Membrane, Microscopy, Nucleotide, Pandemic, Polymerase, Polymerase Chain Reaction, Protein, Respiratory, Reverse Transcriptase, Ribonucleic Acid, RNA, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Spike Protein, Structural Protein, Syndrome, Telomerase, Toxin, Transcription, Translation, Virus

Written by
Pooja Toshniwal Paharia
Dr. based clinical-radiological diagnosis and management of oral lesions and conditions and associated maxillofacial disorders.
Source: Read Full Article