New community-based diagnostic tool is feasible and effective for diagnosing tuberculosis
A new, low-cost, scalable package for diagnosing tuberculosis (TB) onsite in resource-poor community settings is feasible and effective, according to a new trial.
Portable, battery-operated, molecular diagnostic tool, Xpert, was able to detect almost all likely infectious cases of the disease in a community trial of almost 600 participants in South Africa.
Published in Nature Medicine, the findings may signal an important step towards the implementation of active case finding for the disease, helping move diagnostics out of healthcare facilities and into the community.
TB remains a major public health priority globally, responsible for approximately 1.5 million deaths annually in 2020. Although the quality of TB diagnostics has improved considerably over the years, almost 40% of cases still remain undiagnosed and undetected worldwide.
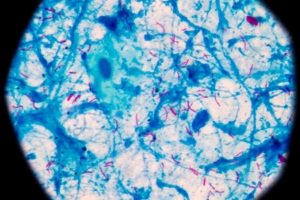
The current global public health strategy for TB centers around passive case finding, which involves patients self-presenting to healthcare facilities when they have symptoms. The standard-of-care in community settings is an older diagnostic methodology known as smear-microscopy (looking for bacteria under a microscope at a local community health center). However, this technique can take several weeks to reach a diagnosis, and being passive means that it may miss out on the considerable amount of TB transmission that occurs prior to diagnosis.
Newer, DNA-based diagnostics are now recommended by the World Health Organization for routine TB diagnosis in endemic countries. These diagnostics, however, are more expensive than smear microscopy and so are often reserved for more difficult-to-diagnose cases. Available evidence on their utility for community-based diagnostics is also limited.
In this open-label, randomized controlled trial (XACT), researchers, including from the London School of Hygiene & Tropical Medicine (LSHTM), compared two diagnostic approaches for TB in the districts of Mitchel's Plain and Klipfontein in Cape Town, South Africa. Both districts have a high burden of informal housing and families living below the poverty line.
A total of 584 participants (median age of 39 years, 65% female) in the community with HIV infection or symptoms of TB were randomly allocated to be diagnostically tested for TB using either same-day smear microscopy or onsite DNA-based molecular diagnosis using Xpert. The XACT mobile clinic model is a relatively low-cost package comprising a vehicle operated by two healthcare workers that contains newer portable battery-operated DNA-based diagnostics, and equipment to obtain sputum samples even when patients cannot produce a sample.
Omics eBook

Overall, although Xpert only picked up about 52% of the case burden of TB in the community, the device detected almost all the likely infectious cases (94.1% compared to 23.5% for smear microscopy). These infectious cases, often called 'super spreaders' are associated with disease transmission and amplification of TB.
Time to treatment initiation for these potentially infectious cases was also substantially quicker with Xpert than with smear microscopy (seven days compared to over three weeks). All patients who tested positive for TB with Xpert were on treatment 60 days later compared to approximately 46% of those diagnosed with smear microscopy.
The authors conclude that these findings emphasize the importance of moving towards an active case finding approach for TB diagnosis, highlighting that portable, DNA-based diagnostic techniques linked directly to care will be important for interrupting transmission of the disease in community settings.
Evidence around the optimum strategy to find TB patients in the community remain sparse and controversial so this study helps fill an important gap.
This scalable approach promises to reduce amplification of the TB epidemic by early diagnosis and rapid treatment initiation of the most infectious cases.
Whilst we focused on two districts in Cape Town, these areas may be representative of many peri-urban shanty towns and 'slums' in Asia, Africa and South America, where there is a high burden of undiagnosed TB. Early community-based diagnosis and initiating treatment interrupts transmission and so prevents amplification of the TB epidemic; we call this active case finding."
Keertan Dheda, Corresponding Author, Professor of Medicine, University of Cape Town and Professor of Mycobacteriology & Global Health at LSHTM
London School of Hygiene & Tropical Medicine (LSHTM)
Esmail, A., et al. (2023) Comparison of two diagnostic intervention packages for community-based active case finding for tuberculosis: an open-label randomized controlled trial. Nature Medicine. doi.org/10.1038/s41591-023-02247-1.
Posted in: Device / Technology News | Disease/Infection News | Healthcare News
Tags: Bacteria, covid-19, Diagnostic, Diagnostics, DNA, Global Health, Healthcare, HIV, Hygiene, Medical Research, Medicine, Microscope, Microscopy, Poverty, Public Health, Research, Tuberculosis
Source: Read Full Article