New computational tool identifies novel targets for cancer immunotherapy

Researchers at Children’s Hospital of Philadelphia (CHOP) and the University of California, Los Angeles (UCLA) have developed a computational platform capable of discovering tumor antigens derived from alternative RNA splicing, expanding the pool of cancer immunotherapy targets. The tool, called “Isoform peptides from RNA splicing for Immunotherapy target Screening” (IRIS), was described in a paper published May 16 in the Proceedings of the National Academy of Sciences.
“Immunotherapy has revolutionized cancer treatment, but for many cancers including pediatric cancers, the repertoire of antigens is incomplete, underscoring a need to expand the inventory of actionable immunotherapy targets,” said co-senior author Yi Xing, Ph.D., director of the Center for Computational and Genomic Medicine at CHOP.
“We know that aberrant alternative RNA splicing is widespread in cancer and generates a range of potential immunotherapy targets. In our study, we were able to show that our computational platform was able to identify immunotherapy targets that arise from alternative splicing, introducing a broadly applicable framework for discovering novel cancer immunotherapy targets that arise from this process.”
Cancer immunotherapy has ushered in a sea change in the treatment of many hematologic cancers, harnessing the power of a patient’s own immune system to fight the disease. Chimeric antigen receptor T-cell (CAR-T) and T cell receptor-engineered T cell (TCR-T) therapies modify a patient’s own T cells to attack known antigens on the surface of cancer cells and have often led to durable responses for cancers that were once considered incurable.
However, the field has encountered challenges in the solid tumor space, in large part due to a lack of known and suitable targets for these cancers, highlighting the need for novel approaches to expand the pool of immunotherapy targets.
Alternative splicing is an essential process that allows for one gene to code for many gene products, based on where the RNA is cut and joined, or spliced, before being translated into proteins. However, the splicing process is dysregulated in cancer cells, which often take advantage of this process to produce proteins that promote growth and survival, allowing them to replicate uncontrollably and metastasize. This happens in many adult and pediatric cancers.
Scientists have suggested splicing dysregulation could be a source of novel tumor antigens for immunotherapy, but identifying such antigens has been a challenge.
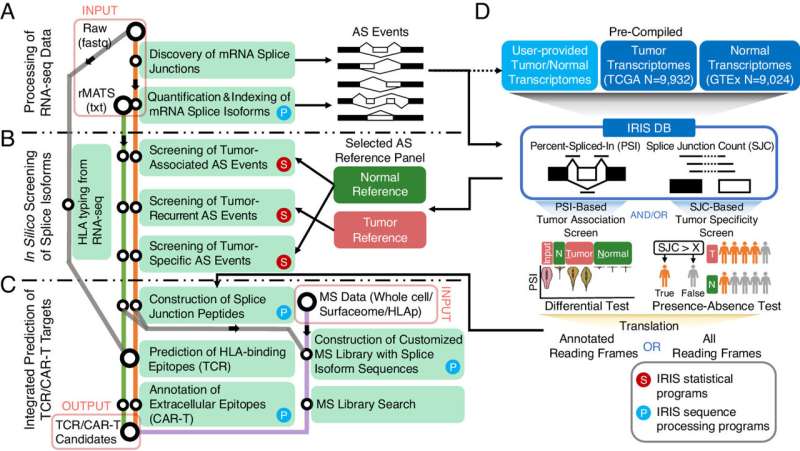
To address this difficulty, the researchers created IRIS to leverage large-scale tumor and normal RNA sequencing data and incorporate multiple screening approaches to discover tumor antigens that arise due to alternative splicing. Integrating RNA sequencing-based transcriptomics data and mass spectrometry-based proteomics data, the researchers showed that hundreds of IRIS-predicted TCR targets are presented by human leukocyte antigen (HLA) molecules, the part of the human immune system that presents antigens to T cells.
The researchers then applied IRIS to RNA sequencing data from neuroendocrine prostate cancer (NEPC), a metastatic and highly lethal disease known to involve shifts in RNA splicing, as discovered in a prior study by CHOP and UCLA researchers.
From 2,939 alternative splicing events enriched in NEPC, IRIS predicted 1,651 peptides as potential TCR targets. The researchers then applied a more stringent screening test, which prioritized 48 potential targets. Interestingly, the researchers found that these targets were highly enriched for peptides encoded by short sequences of less than 30 nucleotides in length—also known as “microexons”—which may arise from a unique program of splicing dysregulation in this type of cancer.
To validate the immunogenicity of these targets, the researchers isolated T cells reactive to IRIS-predicted targets, and then used single-cell sequencing to identify the TCR sequences. The researchers modified human peripheral blood mononuclear cells with seven TCRs and found they were highly reactive against targets predicted by IRIS to be good immunotherapy candidates. One TCR was particularly efficient at killing tumor cells expressing the target peptide of interest.
“Immunotherapy is a powerful tool that has had a significant impact on the treatment of some cancers, but the benefits have not been fully realized in many lethal cancers that could benefit from this approach,” said Owen N. Witte, MD, University Professor of Microbiology, Immunology, and Molecular Genetics and member of the Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research at UCLA.
“The discovery of new antigenic targets that may be shared among different patients—and even different tumor types—could be instrumental in expanding the value of cell-based therapies. Analyzing massive amounts of data on tumor and normal tissues, which requires sophisticated computational tools like those developed by the Xing Lab, provides actionable insights on targets that one day could be tested in the clinic.”
“This proof-of-concept study demonstrates that alternatively spliced RNA transcripts are viable targets for cancer immunotherapy and provides a big data and multiomics-powered computational platform for finding these targets,” Dr. Xing added. “We are applying IRIS for target discovery across a wide range of pediatric and adult cancers. We are also developing a next-generation IRIS platform that harnesses newer transcriptomics technologies, such as long read and single cell analysis.”
More information:
Yang Pan et al, IRIS: Discovery of cancer immunotherapy targets arising from pre-mRNA alternative splicing, Proceedings of the National Academy of Sciences (2023). DOI: 10.1073/pnas.2221116120
Journal information:
Proceedings of the National Academy of Sciences
Source: Read Full Article