New Findings Support DBS in Parkinsons With GBA Mutation
TOPLINE:
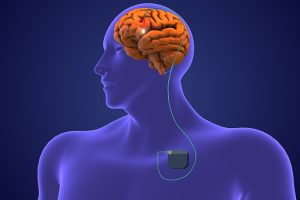
Deep brain stimulation (DBS) for Parkinson’s disease (PD) is as effective in patients with GBA gene mutation as it is in those without this mutation, offering significantly improved motor and nonmotor symptoms, reduced levodopa equivalent daily dose (LEDD) intake, and decreased impulse control disorders (ICDs) for up to 5 years, a new study found.
METHODOLOGY:
-
While DBS has been linked with positive outcomes in patients with PD, its efficacy in patients with GBA mutations (GBA-PD) is less clear.
-
This retrospective, multicenter study included 365 people with PD (mean age 63 years) who underwent mostly bilateral subthalamic nucleus DBS between 2005 and 2021 and genetic testing.
-
Researchers stratified patients into those with a variant of the GBA gene (GBA-PD; 20%) and those without (non-GBA-PD), and classified GBA variants into mild (23.3%) and severe/complex (45.2%).
-
Investigators measured motor and nonmotor outcomes, including cognitive function, LEDD, ICDs, dyskinesias, depression, recurrent falls, and other outcomes in patients at baseline and at 1, 3, and 5 years post-surgery.
TAKEAWAY:
-
At 1, 3, and 5 years post-DBS, both groups had marked improvement in motor symptoms, with a significant reduction in dyskinesias, motor fluctuations, and reduced ICDs, less LEDD intake, and low occurrence of complications such as recurrent falls, depression, hallucinations, and urinary dysfunctions.
-
Patients with GBA-PD had nearly double the prevalence of orthostatic hypotension compared to those without GBA at baseline and 5 years post-surgery.
-
The deterioration of cognitive scores post-DBS and at 5 years was greater with GBA-PD than non-GBA-PD group (25% vs 11%).
IN PRACTICE:
“Our findings support the role of DBS surgery as a valid therapeutic strategy” in patients with PD carrying a GBA mutation, the authors note, as well as the “potential relevance of including GBA testing as part of the diagnostic workout of any patient with PD,” as knowing the GBA genotype could improve clinical management of the disease.
SOURCE:
The study was conducted by Micol Avenali, MD, Department of Brain and Behavioural Sciences, University of Pavia, Pavia, Italy, and colleagues. It was published online October 25 in the Journal of Neurology, Neurosurgery & Psychiatry.
LIMITATIONS:
The study sample was relatively small, and very few subjects received globus pallidus internus (GPi)-DBS, which prevented subgroup comparisons. Some clinical features such as symptomatic orthostatic hypotension were not measured through specific tests or scales, possibly resulting in overestimated or underestimated frequencies. Eight of 73 patients with GBA-PD carried “unknown” variants, the pathogenetic impact of which remains to be determined. The study did not directly measure quality of life.
DISCLOSURES:
The study was supported by grants from the Italian Ministry of Health – Ricerca Corrente 2022-2024 to IRCCS Mondino Foundation and Ricerca di Rete to the Italian Network for Neurosciences and Neurorehabilitation (RIN). The authors report no relevant financial relationships.
Source: Read Full Article