Optimal Timing of Postop Radiosurgery for Brain Metastases
TOPLINE:
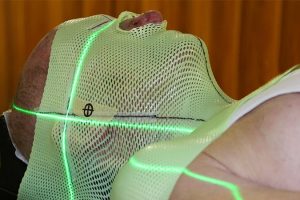
The best time to deliver postoperative adjuvant stereotactic radiosurgery for brain metastases appears to fall within 22 to 30 days after surgery, timing that minimizes both local failure and adverse radiation effects, a new analysis suggests.
METHODOLOGY:
-
Adjuvant stereotactic radiosurgery enhances local control of resected brain metastases, but the optimal timing for this treatment remains unclear. The current study looked at whether stereotactic radiosurgery delivered sooner — within 14 days of surgery — improved local control without increasing adverse radiation effects.
-
Researchers initially compared 61 patients undergoing a rapid adjuvant stereotactic radiosurgery (RapidRT) workflow with 377 historical controls treated using the same dosing and fractionation principles under standard postoperative stereotactic radiosurgery (StanRT) scheduling.
-
The team then evaluated local control, post-treatment adverse radiation effects, and wound complications associated with adjuvant stereotactic radiosurgery delivered 14, 21, and 30 days after surgery.
-
But given the wide variations in time to radiation administration in the StanRT cohort, the authors also combined the patient populations to evaluate the association between timing of radiosurgery and outcomes in all 438 patients.
TAKEAWAY:
-
Local failure and post-treatment adverse radiation effects rates at 1 year were not significantly different between RapidRT and StanRT cohorts.
-
In the overall cohort, local failure rates were highest when stereotactic radiosurgery was given more than 30 days from surgery (10.7%), followed by 22 to 30 days (6.6%), within 14 days (5.1%), and 15 to 21 days (3.2%).
-
The timing of stereotactic radiosurgery was associated with post-treatment adverse radiation effects, with the highest 1-year rates occurring in patients who received stereotactic radiosurgery within 14 days (18.1%), followed by 14 to 21 days (11.1%), more than 30 days (8.7%), with the lowest rate in patients starting radiation 22 to 30 days after surgery (4.1%).
-
Overall survival at 1 year did not differ significantly by timepoint nor did wound complications.
IN PRACTICE:
“This report demonstrates the empirical importance in balancing the benefits of early radiation on local control and the risk of [post-treatment adverse radiation effects], with the optimal timing seeming to occur between 22 and 30 days,” the authors write.
SOURCE:
The study, with first author Evan Bander, MD, from Memorial Sloan Kettering Cancer Center, New York City, was published online October 31 in JAMA Network Open.
LIMITATIONS:
The retrospective study design may lead to confounding biases between groups, which could also affect survival, local failure, or post-treatment adverse radiation effects rates. The study also may not be powered to demonstrate differences in rare events, such as wound complications.
DISCLOSURES:
Funding for the study was provided by the National Cancer Institute. The authors have declared no relevant financial relationships.
Source: Read Full Article