Research finds benefits, risks in state-mandated school-based BMI assessments
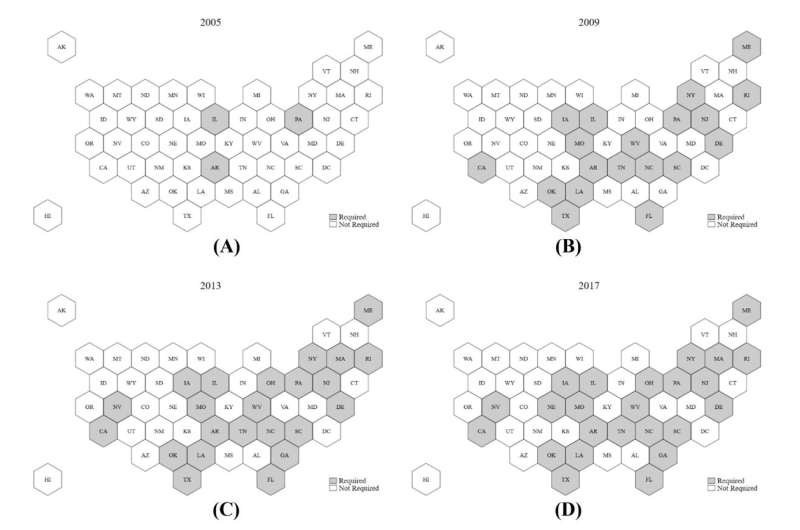
A University of Massachusetts Amherst resource economist finds mandated in-school Body Mass Index (BMI) assessments adopted in varying forms by 24 states to combat childhood obesity have the potential to improve the health of some students while introducing body-image issues for others. The research is believed to be the first to assess these policies as a whole, rather than in single states or school districts.
“In states that passed these laws, overweight and obese teens were more likely to correctly describe their bodies as such, compared to states that do not have these mandates,” says Brandyn Churchill, assistant professor of resource economics at UMass Amherst. “But the unintended consequence is that non-overweight girls were also more likely to describe themselves as overweight. They were less likely to describe themselves as a healthy weight.”
In addition, Churchill finds that overweight teenagers were more likely to report that they were trying to lose weight. He identifies a small but significant decrease in teens’ BMI.
“These changes appear to be coming from students who were right on the margin of being overweight,” he says.
The study did not detect any meaningful changes in exercise or calorie-limiting behaviors linked to mandated BMI assessments. The findings are based on national and state Youth Risk Behavior Surveys between 1991 and 2017.
Churchill points out that the average BMI of children in the U.S. has been steadily increasing over that span, even as more states enacted mandatory assessments.
“It’s hard to look at the change in childhood BMI and say these policies are a resounding success, given the potential unintended consequences for adolescent girls in the form of distorted self-image and body perception,” he says. Prior research has found these issues can lead to shame, anxiety, bullying and eating disorders.
While tracking the BMI of children may be a helpful measure in assessing the overall health of young people and even the health of students in each school, Churchill finds there’s little evidence that it helps individual students adopt healthier habits. Despite their use by so many states, BMI assessments do not meet American Academy of Pediatrics guidelines for routine health screenings.
“Focusing on ways to encourage or incentivize healthy weight-management practices is beneficial, relative to just telling kids to eat small portions and that they’re overweight,” Churchill notes.
He concludes it is ultimately up to policymakers to consider the benefits and costs of mandated BMI assessments in schools.
“Are they comfortable with a little more awareness for the overweight kids at the expense of the self-image of the non-overweight girls?” Churchill asks. “That’s a policy choice. They have a hard job.”
The full paper appears in the latest edition of the Journal of Policy Analysis and Management.
More information:
Brandyn F. Churchill, State‐mandated school‐based BMI assessments and self‐reported adolescent health behaviors, Journal of Policy Analysis and Management (2023). DOI: 10.1002/pam.22523
Journal information:
Journal of Policy Analysis and Management
Source: Read Full Article