SARS-CoV-2 South Africa and Brazil variants show resistance to therapeutic antibodies

A team of scientists from Germany has determined the efficacy of currently used therapeutics in treating newer variants of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), including the B.1.1.7 (UK), B.1.351 (South Africa) and B.1.1.248 (Brazil) variants. Their findings reveal that both B.1.351 and B.1.1.248 variants are able to escape humoral immune responses induced by therapeutic antibodies, vaccinations, or natural SARS-CoV-2 infection. The study is currently available on the bioRxiv* preprint server.
Background
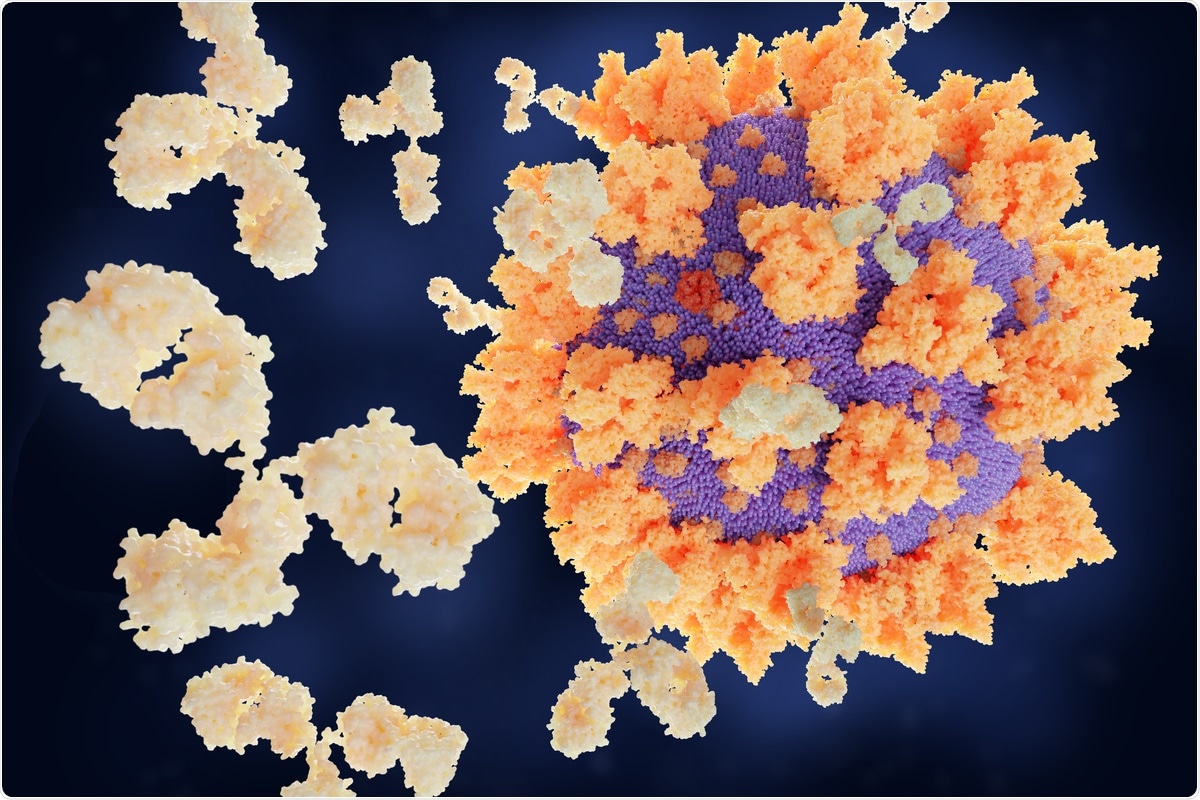
Since its emergence in December 2019, the highly infectious and lethal SARS-CoV-2, the causative pathogen of coronavirus disease 2019 (COVID-19), has infected more than 108 million people and claimed more than 2.3 million lives globally. In a global effort to control the viral spread, many studies have been done in the search for effective therapeutic strategies against COVID-19. Currently, several repurposed antiviral medicines and therapeutic antibodies are being used to treat critical COVID-19 patients. As a protective measure, some potential vaccines targeting the viral spike protein have received emergency use approval from concerned authorities.
In the later phase of the pandemic, several new variants of SARS-CoV-2 have been emerged, including B.1.1.7 (UK), B.1.351 (South Africa), and B.1.1.248 (Brazil) variants. Several mutations found in the spike protein of these variants have been found to significantly increase their infectivity. Moreover, there are preliminary studies suggesting that these variants may be more virulent and are likely to increase the COVID-19-related mortality rate. Because the majority of currently available therapeutic antibodies and vaccines primarily target the spike protein of SARS-CoV-2, potential concerns are rising about the effectiveness of current therapeutic interventions in preventing the spread and lethality of newly emerged variants.
In the current study, the scientists have evaluated the efficacy of viral entry inhibitors, monoclonal antibodies, and vaccines in preventing infections by the UK, South Africa, and Brazil variants of SARS-CoV-2.
Study design
The scientists used both human and animal cell lines to conduct in vitro experiments. To analyze the effectiveness of viral entry inhibitors against the SARS-CoV-2 variants, they used soluble angiotensin-converting enzyme 2 (ACE2), cellular protease (TMPRSS2) inhibitors, and membrane fusion inhibitors (EK1 and EK1C4). To determine whether these variants are resistant to host humoral immune responses, the scientists thoroughly analyzed the efficacy of anti-SARS-CoV-2 antibodies obtained from three different types of sources: 1) therapeutic monoclonal antibodies (Casirivimab, Imdevimab, and Bamlanivimab); 2) plasma samples collected from critically ill COVID-19 patients; and 3) serum samples collected from people vaccinated with BioNTech/Pfizer vaccine (BNT162b2).
Important observations
Although there is evidence suggesting increased transmissibility of recently emerged SARS-CoV-2 variants, the current study scientists did not observe any significant differences in host cell entry dynamics between the wildtype virus and the UK, South Africa, and Brazil variants. Specifically, the spike proteins of wildtype and all tested variants of SARS-CoV-2 showed comparable efficiency in entering host cells.
Interestingly, the entry of both wildtype and mutated variants into the host cell was significantly blocked by soluble ACE2, TMPRSS2 inhibitor, and membrane fusion inhibitors. Compared to the wildtype virus, the variants showed higher susceptibility to soluble ACE2-mediated inhibition. Similarly, the Brazil variant showed higher susceptibility toward membrane fusion inhibitors. These observations indicate that viral entry inhibitors may be potentially used to prevent infections mediated by mutated variants of SARS-CoV-2.
Despite showing comparable host cell – virus interaction dynamics, significant differences in antibody-mediated neutralization were observed between the wildtype virus and the mutated variants. Among tested monoclonal antibodies, Imdevimab showed comparable efficacy in inhibiting host cell entry by all viral variants. In contrast, both South Africa and Brazil variants showed partial and complete resistance toward Casirivimab and Bamlanivimab. However, all tested antibodies showed high potency in inhibiting the UK variant.
Neutralizing antibodies generated in response to SARS-CoV-2 infection are expected to provide protection against reinfection. To determine the efficacy of convalescent plasma therapy against viral variants, COVID-19 patient-obtained plasma samples with high wildtype spike protein neutralizing efficacy were tested against all viral variants. The findings revealed that host cell entry via the spike protein of the South Africa and Brazil variants was less efficiently inhibited by the majority of plasma samples tested. This indicates that people previously infected with wildtype SARS-CoV-2 are only partially protected against South Africa and Brazil variants.
Regarding vaccine-mediated protection, the findings revealed that most of the serum samples obtained from BNT162b2-vaccined people had lower efficiency in inhibiting spike-driven host cell entry compared to that observed for the wildtype SARS-CoV-2 and the UK variant.
Study significance
The study reveals that current therapeutic interventions are less effective in inhibiting South Africa and Brazil variants of SARS-CoV-2, and thus, strict implementation of non-pharmaceutical control measures is required to contain their transmission.
*Important Notice
bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Markus Hoffmann et al. 2021. SARS-CoV-2 variants B.1.351 and B.1.1.248: Escape from therapeutic antibodies and antibodies induced by infection and vaccination. BioRxiv. doi: https://doi.org/10.1101/2021.02.11.430787, https://www.biorxiv.org/content/10.1101/2021.02.11.430787v1
Posted in: Medical Science News | Medical Research News | Disease/Infection News | Healthcare News
Tags: ACE2, Angiotensin, Angiotensin-Converting Enzyme 2, Antibodies, Antibody, Cell, Convalescent Plasma, Coronavirus, Coronavirus Disease COVID-19, Efficacy, Enzyme, Immunology, in vitro, Mortality, Pandemic, Pathogen, Protein, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Spike Protein, Syndrome, Therapeutics, Vaccine, Virus

Written by
Dr. Sanchari Sinha Dutta
Dr. Sanchari Sinha Dutta is a science communicator who believes in spreading the power of science in every corner of the world. She has a Bachelor of Science (B.Sc.) degree and a Master's of Science (M.Sc.) in biology and human physiology. Following her Master's degree, Sanchari went on to study a Ph.D. in human physiology. She has authored more than 10 original research articles, all of which have been published in world renowned international journals.
Source: Read Full Article