Study finds the mechanism used by metastatic cancer cells to infiltrate the liver
Metastasis—when cancer spreads to form new tumors—causes approximately 90% of cancer-related deaths. Because metastatic cancer cells circulate in the blood, the liver—which filters the blood—is considered the most vulnerable organ, so treatments that prevent liver metastasis are urgently needed. A team of Osaka Metropolitan University researchers discovered a mechanism that allows metastatic cancer cells to infiltrate the liver, and how that infiltration can be blocked by inhibiting a related protein.
Approximately 90% of cancer-related deaths are due to metastasis when cancer spreads and forms new tumors. The liver is considered the most vulnerable organ to metastatic cancer: the 5-year survival rate after surgery to remove liver metastases is as low as 30–50%, so developing treatments to prevent liver metastasis is urgently needed.
A group of researchers, including graduate student Truong Huu Hoang and Professor Norifumi Kadawa from the Osaka Metropolitan University Graduate School of Medicine, and Associate Professor Misako Matsubara from the Graduate School of Veterinary Science, has identified an alternative pathway for liver metastasis, showing that cancer cells invade via intracellular gap formation in endothelial cells, and clarified the molecular mechanism involved. The results of their research are expected to lead to the development of drugs to prevent and treat metastatic liver cancer.
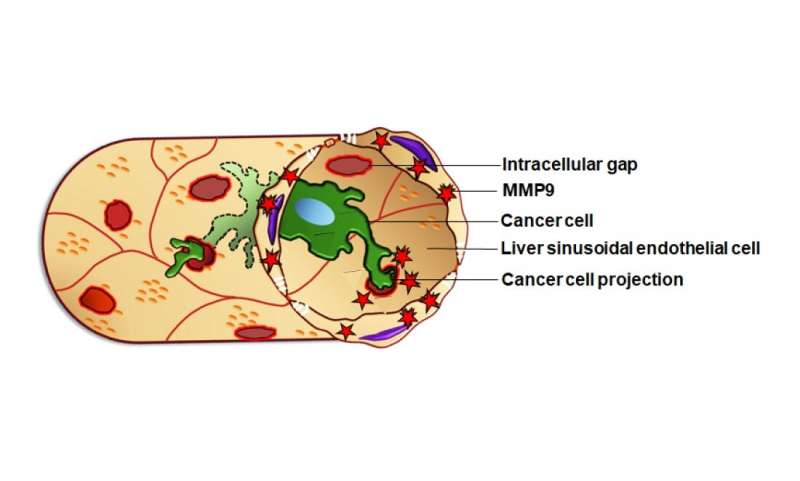
Metastasizing cancer cells are known to change the microenvironment of liver cells in ways that promote metastasis, but the extent of these interactions has not been fully investigated. Cancer cells carried in the bloodstream come into contact with liver sinusoidal endothelial cells (LSECs), which line the blood vessels of the liver to form a protective barrier.
LSECs are responsible for the detoxification functions of the liver and have numerous small pores, through which the liquid components of blood and small particles—but not cancer cells—can enter the liver. LSECs are constantly exposed to toxic substances carried by the blood that can disrupt these small pores under stressful conditions; this causes larger intracellular gaps to form in the LSECs, weakening the protective barrier. This led the research group to consider that the LSECs’ intracellular gaps may be involved in liver metastasis.
The research group created a mouse model of liver metastasis—by injecting cancer cells into the spleen—and performed omics analysis to observe changes in the LSECs. They found that when cancer cells moved from the spleen to the liver, they induced the LSECs to produce multiple proteins. The expression of one of these proteins—matrix metalloproteinase 9 (MMP9)—in LSECs caused the intracellular gaps to form.
Furthermore, using electron microscopy and 3D tomography reconstruction, the researchers showed that cancer cells extended their projections directly into the intracellular gaps of LSECs, allowing them to infiltrate the liver tissue. They found a positive correlation between the number of intracellular gaps in the LSECs and the number of new metastatic liver tumors that formed in the mice. However, new tumors could be prevented from forming by treating the mice with a MMP9 inhibitor, suggesting that MMP9 is a promising therapeutic target to prevent liver metastasis.
Professor Matsubara concluded, “In this study, we discovered a new phenomenon related to metastasis: cancer cells induce LSEC intracellular gap formation and infiltrate the liver through those gaps. With these results we are continuing our research to develop new treatments for liver metastasis, targeting intracellular gap formation in LSECs.”
Source: Read Full Article