Systematic study of free fatty acids reveals new roles in metabolic diseases

Researchers have developed a technology, FALCON, to analyze the effects of free fatty acids in any cell type, and found type 2 diabetes genes that may further boost diabetes risk when cells are in a high-fat environment.
High levels of fat molecules called free fatty acids in the bloodstream are a common risk factor for several diseases, including type 2 diabetes and cancer. Learning how fatty acids interact with cells in the body could help researchers to better understand the biological mechanisms that lead to disease and to develop new treatments. However, until recently, there was no way to systematically study the effects of diverse fatty acids in cells.
Now researchers from the lab of Anna Greka, an institute member at the Broad Institute of MIT and Harvard, have developed a platform called FALCON (Fatty Acid Library for Comprehensive ONtologies) that can systematically profile the effects of a wide range of different free fatty acids in any cell type of interest, including cellular models of disease.
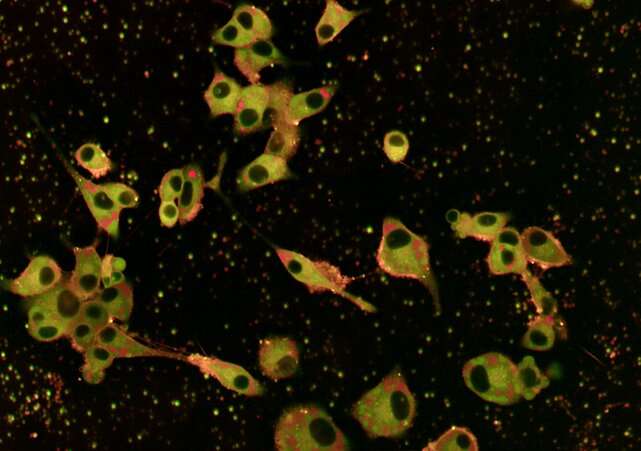
The method, described in a study in Cell Metabolism, allows scientists to expose cells to a large number of free fatty acids, mimicking conditions in the body, and to measure changes in the cells’ gene activity, shape or morphology, survival, fat composition, and other key characteristics.
Using their method on human pancreatic beta cells, a cell model for type 2 diabetes, the scientists found that some monounsaturated fatty acids—long thought to be beneficial for health—are actually toxic to cells. The finding suggests that traditional ways of classifying fatty acids may not accurately reflect what the molecules do to cells in health and disease. Based on their data, the team came up with a new way to classify the molecules.
And by broadly surveying gene activity in the cells as they were being exposed to, or “perturbed” by, the fatty acids, the scientists also identified genes linked to type 2 diabetes risk that showed altered activity after fatty acid exposure. The scientists said that those genes might explain how high fat levels in the blood can boost diabetes risk in those who are genetically susceptible to the disorder.
Moreover, because FALCON analyzed the effects of a large library of fatty acids at once, the team was able to zero in on one gene that helps regulate the toxic effects of the molecules. Other methods had not identified this gene because they either looked at genetic risk alone without taking into account the effects of lipids (fat molecules), or they used only one fatty acid, palmitic acid, as a representative of toxic lipids.
“FALCON has allowed us to integrate the effects of environmental exposure and genetic risk to gain new insights into the mechanisms of metabolic disease. Without this approach, we would have not discovered key regulators that are operative only at the nexus of genes linked to diabetes and the lipid environment that cells are exposed to,” said Juliana Coraor Fried, an MD/Ph.D. student at Broad, Harvard Medical School, and MIT and co-first author on the study.
“The idea behind this study was to develop a systematic approach to study the phenotypes that are induced by different fatty acids in any cell type of interest. We are thrilled that FALCON is already inspiring others to explore this concept in their own systems,” said Nicolas Wieder, a co-first author on the paper and a visiting postdoctoral fellow at the Broad.
Many collaborators from Broad and other institutions contributed to the work, including Broad institute member Beth Stevens, who is also an associate professor at Harvard Medical School and an investigator at Boston Children’s Hospital, and Broad institute scientist Anne Carpenter, who is also senior director of the Imaging Platform and co-developer of Cell Painting, an image-based cell profiling technique that is part of the FALCON platform.
A technique takes flight
Previous studies tested only a few fatty acids one at a time, so the Greka lab set out to develop FALCON to study them at scale. To do this, Wieder, Coraor Fried, and colleagues overcame an important hurdle: they figured out a way to deliver fatty acids, which aren’t soluble in water, to cells using existing high-throughput systems and at concentrations similar to those found in human blood.
“Our group studies fundamental cellular mechanisms using scalable methods, with a particular interest in membrane proteins. We still do not understand how proteins interact with the lipids in their neighborhood to regulate their behavior, because lipids are hard to study, especially at scale. This gap in our scientific knowledge was the inspiration for FALCON,” said Greka, the senior author of the study, who is also an associate professor at Harvard Medical School and a physician at Brigham and Women’s Hospital.
The researchers used FALCON to study the effects of 61 fatty acids in human pancreatic beta cells. They found that 20 of the molecules led to toxic effects that mirrored those associated with type 2 diabetes.
More than half of these were monounsaturated fatty acids that had surprising effects on cells. For example, some were even more toxic than saturated fatty acids, by increasing rigidity of cell membranes. And some fatty acids showed varying levels of toxicity in different cell types.
“Monounsaturated fatty acids are not one group of fatty acids that induce similar phenotypes” said Coraor Fried. “There are some that seem neutral or protective, while there’s a whole group of monounsaturated fatty acids that seems to be toxic.” She added that this finding opens a new avenue of research into the actions of fatty acids in different cell types and disease models.
The team found 25 genes previously associated with risk of type 2 diabetes that were also altered by fatty acid exposure. One gene, GLP1R, is a well-known drug target for type 2 diabetes and obesity—a finding the scientists said is a cross-validation of the FALCON approach.
Another gene, CMIP, had never been flagged before as a key regulator in either pancreatic beta cell biology, which is relevant to diabetes, or in conditions marked by dysregulated lipids in the blood. But through the use of FALCON, the team showed CMIP protects pancreatic beta cells from the toxic effects of fatty acid exposure.
FALCON’s future
The authors said researchers can apply the FALCON protocol to any cell type affected by fatty acids. For example, their paper showed how certain fatty acids were toxic to microglial cells, which are implicated in Alzheimer’s disease. Other Broad researchers have begun using FALCON to study fatty acid effects in fat cells, neurons, and immune cells.
Wieder and Coraor Fried added that discoveries made using FALCON will open doors to a better understanding of disease progression. It could also have implications for future therapies.
“One idea is to use a fatty acid profile measured in the blood of patients as a tool for individualized or personalized medicine,” said Wieder. “As long as you can come up with a cellular model that’s relevant for the disease you want to study and that has lipids as an environmental risk factor, you can just plug it in and start exploring.”
More information:
Nicolas Wieder et al, FALCON systematically interrogates free fatty acid biology and identifies a novel mediator of lipotoxicity, Cell Metabolism (2023). DOI: 10.1016/j.cmet.2023.03.018
Journal information:
Cell Metabolism
Source: Read Full Article