para que sirve meloxicam metocarbamol generico
Psychotherapy is one of the two main treatments for posttraumatic stress disorder (PTSD). The other is pharmacologic therapy, and selective serotonin reuptake inhibitors (SSRIs) are the first-line treatment. With this approach, however, response rates rarely exceed 60%, and fewer than 20% to 30% of patients achieve full remission.
But new strategies bring hope to individuals who suffer from the condition. In a study published in March in SAGE Open Medicine, researchers from the Federal University of Santa Maria (UFSM), Santa Maria, Rio Grande do Sul, Brazil, paxil interactions with tramadol reported that adjuvant transcranial direct current stimulation (tDCS) can be an alternative treatment for refractory PTSD. The patients in the study were survivors of one of the deadliest nightclub fires in history, and the deadliest ever to have occurred in Brazil.
The KISS nightclub fire broke out in the early morning hours of Sunday, January 27, 2013, killing 242 people. Over a decade later, the hundreds of individuals who survived the tragedy continue to experience not only physical effects but also psychological effects. Among the most common is PTSD.
One of the places the survivors can turn to for help is the Integrated Center for Attention to Victims of Accidents, which was established at Santa Maria University Hospital in the wake of the fire. It was from this center that the study’s patients were recruited.
Although 145 patients were screened, only eight met the inclusion criteria. They were older than 18 years, had been diagnosed with PTSD without complete remission of symptoms, and had maintained their pharmacologic treatment schedule without unchange during the 3 weeks before the beginning of the proposed treatment and during the proposed treatment.
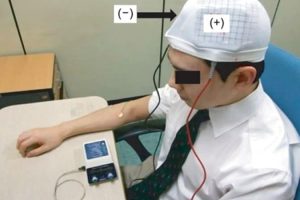
Over the course of 10 days, each participant underwent one daily 30-minute tDCS session in which a current of 2 mA was used for an area of 25 cm2.
The following four standardized scales were used to assess the participants: the Post-Traumatic Stress Disorder Checklist – Civilian Version, the Montreal Cognitive Assessment, the Hamilton Depression Rating Scale, and the Hamilton Anxiety Rating Scale. The scales were applied before tDCS, after tDCS, at 30 days post intervention, and at 90 days post intervention.
The investigators found that after adjuvant treatment with tDCS, the patients experienced improvement of 20% in the central symptoms of PTSD, 60% in depressive symptoms, and 54% in anxious symptoms. Despite a decrease in these effects over time, this improvement was maintained throughout the first month after treatment.
The participants’ cognition also improved. The improvement occurred slowly and progressively and became statistically significant at the end of the first month of treatment.
All the researchers were from the UFSM. They included Kathy Marcolin, MD; Ângelo da Cunha, MD, PhD; Beatriz Yoneyama, MD; and Tiango Ribeiro, MD, PhD. In an interview with Medscape Portuguese Edition, they said that many findings caught their attention — above all, that the improvement was maintained. Given that this improvement occurred among individuals whose condition was refractory to pharmacologic treatment, the researchers think that the intervention may yield even better outcomes for patients with other conditions.
“We can infer that patients with less intense symptoms could have an even more positive response. In addition, by carrying out tDCS according to an established maintenance schedule, we could see the attained benefits last even longer.”
The benefits were quite pronounced, and the adverse effects (mainly local hyperemia, pruritus, mild discomfort, and headache) were minor and brief.
The team pointed out that, owing to the study’s small sample size, the findings, while encouraging, cannot be extrapolated to other populations. “Nevertheless, the positive results we obtained serve as an incentive to follow up on the research using larger sample sizes.” Moreover, tDCS is a low-cost, effective, flexible, and well-tolerated technique. It thus is a promising therapeutic tool that can be used in doctors’ offices throughout Brazil.
The technique has already been proven to be a safe and well-tolerated alternative for other conditions as well. “Studies have shown, for example, that tDCS is superior to placebo in treating major depressive disorder, a very common illness that has significant direct and indirect costs,” say the researchers. Positive results have been reported for individuals with alcohol use disorder. Patients with schizophrenia have also benefited from tDCS, especially in terms of reducing auditory hallucinations. The technique has been successful as a treatment for chronic pain and migraine and as an approach to neurologic rehabilitation.
Yet, despite these positive reports, tDCS is still mostly used within research-specific protocols. According to the UFSM team, more studies are needed before the technique can become part of regular clinical practice. Regarding the treatment of PTSD, for example, in-depth research should be carried out on aspects related to long-term effects, the positioning of electrodes, and the standardization of the application area.
This article was translated from the Medscape Portuguese Edition.
Source: Read Full Article