Is there a genetic link between the risk of schizophrenia and the surface of the brain?
Schizophrenia is a severe brain disorder. Worldwide, it affects about one in a hundred people in their lifetimes. No one knows exactly why some people develop schizophrenia, but it is known that a combination of biological and environmental factors contributes to the disease. Among biological factors, genes play an important role. Twin studies have shown that genetic factors account for about 80 percent of an individual’s risk of developing schizophrenia.
However, do the same genes that influence the risk of developing schizophrenia also affect biological characteristics of the brain that we can measure? According to a new study, there is indeed a genetic association between the risk of schizophrenia and the surface of the brain.
“The results of our study demonstrate that a group of genes that contribute to the risk of schizophrenia also affect the thickness and size of the brain’s surface,” Weiqiu Cheng says. She is a Postdoctoral Fellow at the Norwegian Centre for Mental Disorders Research, NORMENT.
The study paves the way for new insight into the brain of people with schizophrenia
The surface of the brain is the outermost layer of the brain. This layer is called the cerebral cortex, primarily constructed of gray matter. It consists of around 20 billion nerve cells that are tightly packed together. This area is involved in multitudinous high-level brain functions, such as emotion and reasoning.
What do we refer to when we speak about the thickness and size of the surface of the brain?
Imagine that our brain is like a sheet of paper crumpled into a ball. When we speak about the thickness of the surface of the brain, we refer to the thickness of the sheet itself. The size of the surface of the brain is the surface area of the sheet, which is the same whether the sheet is lied out flat or curled.
These characteristics of the brain thus seem to be influenced by a group of genes that also contribute to the risk of schizophrenia.
“In previous studies, researchers found that patients of schizophrenia showed significant differences in the thickness and size of the surface of the brain, compared with healthy people. Our study may provide biological insights into these findings,” Cheng says.
The thickness and size of the surface of the brain may be promising biomarkers
For a long time, researchers have tried to find out if there are so-called biomarkers for mental disorders such as schizophrenia. A biomarker for schizophrenia would mean that we could determine someone’s risk of schizophrenia based on one or more measurable biological characteristics.
“Today, it is not possible to determine conclusively whether someone has schizophrenia based on medical examinations. We want to find out if there is a reliable and objective biomarker, i.e., one or more biological characteristics, that are associated with the risk of schizophrenia,” Weiqiu Cheng states.
She adds, “The thickness and size of the surface of the brain can potentially be such biomarkers.”
The findings from the present study may be a small step towards this endeavor.
“The genetic overlap that we found help us understand the genetic relationship between schizophrenia and the thickness and size of the surface of the brain. This may pave the way for future biomarker studies of schizophrenia,” Cheng points out.
Cortical folding and sulcal depth are also hereditary
Researcher Dennis van der Meer also works at NORMENT. He has recently published a study in which he looks at another parameter, namely the folding of the human cerebral cortex measured by sulcal depth.
To explain what sulcal depth means, we must return to the example where we look at the brain as a sheet of paper. When we crumple the sheet like a ball, there will be some folds and bumps. Sulcal depth is the depth of the various folds and bumps of the ball.
“Surprisingly, few researchers have looked at this parameter so far,” van der Meer says.
Dennis van der Meer and his colleagues found that sulcal depth is largely determined by our genes.
“This suggests that sulcal depth can be an interesting feature to investigate further. I am very excited about what we may find out in the future,” he says. “We already found out that some of these genes are also involved in brain disorders, including schizophrenia. This indicates that this under-investigated brain feature can provide many leads on how these disorders come about.”
A biomarker can contribute to better prevention, diagnosis and treatment in the future
Today, the schizophrenia diagnosis is given based on systematic interviews and questionnaires.
“Schizophrenia is a highly heterogeneous mental disorder. This means that patients with schizophrenia vary widely in their symptoms, course of illness and outcome,” Cheng says.
People with schizophrenia also suffer an increased prevalence of other mental disorders.
“Today’s diagnostic methods are therefore demanding and time-consuming both for patients and for clinicians. If, on the other hand, the diagnosis can be formulated based on a biomarker, linked to, for example, the brain or genes, then it is more objective and less demanding,” Weiqiu Cheng explains.
She believes that a biomarker for schizophrenia could also contribute to better prevention and treatment.
The study from NORMENT is the first to demonstrate the genetic overlap
Researchers have long believed that there is a genetic link between different structures in the brain and schizophrenia. Nevertheless, the study from NORMENT is the first to be able to prove the genetic overlap.
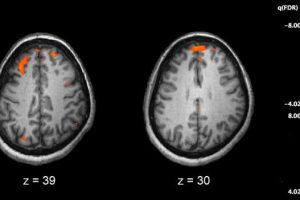
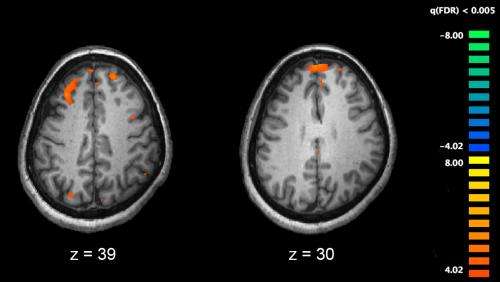
“In previous studies that I referred to earlier, researchers looked at MRI images of the brain of people with schizophrenia. They revealed that people with schizophrenia had some unusual changes in the structure of the brain. This was when the researchers discovered that the thickness and size of the surface of the brain were different from healthy people. However, the researchers were not able to prove the genetic overlap statistically,” Weiqiu Cheng explains.
Cheng and her colleagues at NORMENT therefore chose to use another analytic method than those used in previous studies. In total, they analyzed the genes of more than 40,000 people with schizophrenia and almost 65,000 healthy people, through large European databases. This is how they proved the genetic link.
“I want to continue in this field and believe that genetic studies of this type may ultimately help us understand why some people get schizophrenia and how the disorder develops over time,” Weiqiu Cheng concludes.
Source: Read Full Article