GPs told not to use language that could belittle patients
GPs are urged not to use language that could belittle patients: Doctors should stop using phrases like ‘sending’ home patients who present a ‘complaint’
- Cambridge doctors warned medics not to use words like ‘send’ patients home
- They said language that ‘belittles or blames patients’ is overdue for a change
- Childlike language is particularly common with conditions like diabetes
Woke medics are calling for a revamp of language used by doctors so it does not ‘belittle’ patients.
Common medical phrases like ‘take’ a test or ‘send’ someone home may potentially make patients feel ‘childlike’, they said.
Instead of saying things like the patient ‘denies’ chest pain, doctors should use the word ‘reports’ so it does not sound like the patients is being doubted.
Saying medication ‘failed’ to work implies it was the patient’s fault so doctors should say a drug was ‘not effective’ instead.
The recommendations were made by consultant physician Dr Zoe Fritz and junior doctor Dr Catriona Cox, both from the University of Cambridge.
They laid out an argument for more empowering language in an editorial published in the British Medical Journal (BMJ).
The changes are ‘not a matter of political correctness’, the medics argue.
Simple words or phrases, both verbally and in written notes, can ‘insidiously’ affect the relationship between doctors and their patients, they claim.

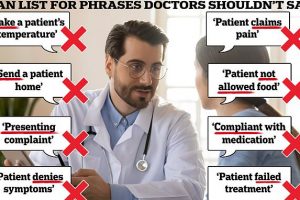
Woke doctors are calling for a revamp of the language used by medics at appointments so it does not belittle patients. Graphic shows: Phrases University of Cambridge doctors said medics should not use

Doctors were today told not to belittle patients by using childlike language such as saying they will ‘send’ them home
Words like ‘send’ a patient home or ‘take’ a patient’s temperature emphasise the doctor’s position of power and may seem patronising, they said.
To say that a patient presented with a ‘complaint’ also carries negative connotations, the medics argue. Words like ‘problem’ or ‘concern’ should be used instead because they are more sympathetic to patients.
Much of the language highlighted here is deeply ingrained in medical practice and is used unthinkingly by clinicians, Dr Fritz and Dr Cox write.
Doctors will have a duty to respect a patient’s wishes for face-to-face appointments under new guidance from the medical regulator.
It says medics should agree with a patient what type of appointment would best suit their ‘needs and circumstances’.
And they should ensure care is ‘safe and effective’ whether delivered face to face or remotely, the General Medical Council says.
The new directive is included in a revised version of the GMC’s core guidance for all doctors, known as ‘Good medical practice’.
It is the modern day equivalent of the Hippocratic Oath, outlining the professional values, knowledge and behaviours expected of UK doctors.
The 16-page document is being updated for the first time since 2013 to reflect societal changes, including sexual harassment and the increased use of social media.
Clinicians should consider how their language affects attitudes and choose language that facilitates trust, balances power, and supports shared decision making, they said.
It comes amid a huge row over the working hours of family doctors, the ‘postcode lottery’ of GP access and face-to-face appointments.
The General Medical Council — which regulates doctors — waded into the row yesterday, telling doctors they have a duty to respect a patient’s wishes for face-to-face appointments in new guidance.
GPs should agree with a patient what type of appointment would best suit their ‘needs and circumstances’, the new guidance says.
In their editorial, Dr Cox and Dr Fritz suggested doctors should address patients with more respect.
Language that suggests a patient is childlike is particularly common with conditions like diabetes, they said, highlighting the term ‘poorly-controlled diabetes’ used to describe someone with consistently high blood-sugar levels.
‘Patients do not like many of these commonly used phrases, and some are associated with problematic changes in the attitudes of healthcare workers.’
Terms like ‘compliance’ and ‘non-compliance’ with medication are authoritarian, the authors claimed.
They wrote: ‘There is an authoritarianism, for example, in talking about patients not being “allowed” certain foods by their doctors.
‘Although patients can find such language upsetting or frustrating, some also adopt a childlike narrative, describing the effect of being “naughty” or “good” on their blood sugars, or recounting being ‘scolded’ by healthcare professionals.’
Phrases such as ‘denies chest pain’ should be replaced with ‘reports no chest pain’, they said.
The authors said: ‘Language that belittles, infantilises, or blames patients runs counter to the collaborative relationships we are trying to foster through initiatives such as shared decision making.
‘We encourage all to reflect on the words and phrases currently used in practice, in particular considering whether they hamper or help to establish a genuinely collaborative therapeutic relationship.’
Source: Read Full Article