HIV Prevention: Clinician Attitudes May Be Curtailing PrEP Use

Taking an antiretroviral tablet daily for preexposure prophylaxis (PrEP) has been shown to be a safe and effective method of HIV prevention. However, low and variable uptake of PrEP among men who have sex with men (MSM) remains concerning.

Dr Samuel Bunting
Clinician attitudes appear to be one of the barriers to PrEP use, according to a new study published in the Journal of Acquired Immune Deficiency Syndrome. Lead author Samuel R. Bunting, MD, and colleagues explored whether the attitudes of prescribing clinicians are impeding access to PrEP among MSM in the United States. They sought to understand whether clinician biases and expectations about race, HIV risk, adherence, and condom use might be affecting willingness to prescribe PrEP to a patient who specifically requests it.
They reached out to 16 US medical schools (allopathic and osteopathic) with a combined total of 12,660 students. A total of 1592 students indicated interest in participating in the study, and 600 completed it accurately.
Researchers simulated an electronic medical record for a fictional patient: a sexually active cisgender MSM presenting to a primary care physician and directly requesting access to PrEP for the first time. The simulated record included an uncomplicated medical history and lab results indicating that the patient was negative for HIV and other STIs.
Researchers systematically varied key aspects of the fictional patient, including his race (White or Black) and his intentions for future condom use if prescribed PrEP (continue using, unlikely to begin using, or will stop using). They asked the medical students a series of questions about their hypothetical patient interaction, including assessing patient HIV risk and provider willingness to prescribe PrEP.
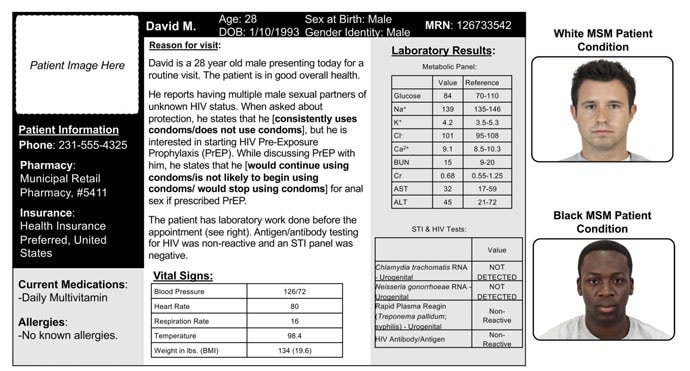
The simulated medical records randomly included Black and White patients.
Bunting and coauthors found that the medical students were significantly less likely to indicate that they would prescribe PrEP to a patient described as “intending to discontinue” condom use were he to be prescribed PrEP, compared with patients “intending to continue” former practices of condom use or non-use. On a scale from 1 (least likely to prescribe) to 7 (most likely to prescribe), willingness to prescribe was highest for the continued-nonuse group (mean score 6.35; 95% CI, 6.18 – 6.52) and was lower for the planned-discontinuation group (mean score 5.91; 95% CI, 5.75 – 6.08; P = .001).
This finding reflects a prevailing fear of “risk compensation” — the concern that an individual on PrEP may start to take additional compensatory risks in his HIV exposures, including discontinuing condom use or increasing number of sexual partners.

Dr Julia Marcus
In an interview with Medscape Medical News, Julia Marcus, PhD, MPH, an associate professor in the Department of Population Medicine at Harvard Medical School and Harvard Pilgrim Health Care Institute, Boston, said: “These provider concerns [about risk compensation] are missing the mark. Just like oral contraception, the whole point of a prevention tool like PrEP is to allow people to engage in certain behaviors more safely. Rather than an unwanted consequence, behavior change may be the intended goal.” Marcus was not involved in the study.
Prior research has shown that uptake of PrEP among Black MSM is significantly lower than among White MSM in the United States. But this study showed no associations with patient race. However, Bunting and his coauthors found a troubling association with the personal attitudes of the medical students toward sexual activity: the more likely the medical students were to disapprove of non-monogamy, the more likely they were to assume the possibility of future nonadherence to PrEP and to hesitate before prescribing PrEP.
Were the medical students making assumptions about patients’ ability to be faithful and consistent, whether to a partner or to a drug regimen? Either way, provider hesitancy to prescribe PrEP to a patient on the basis of their stated intention to discontinue condom use or because of the clinician’s own internalized biases about nonmonogamous relationships both represent troubling barriers to accessing clinical care, reinforcing the clinician’s role as gatekeeper to PrEP.
“It’s frustrating that these biases are still in play and potentially contributing to slow and inequitable PrEP uptake” Marcus commented. “Every sexually active primary care patient should be informed about PrEP, in accordance with CDC guidance, but providers often feel constrained by time…We need tools that can normalize PrEP in primary care and help limit the potential effect of biases on PrEP prescribing decisions.”
In an interview, Bunting, resident physician in the Department of Psychiatry and Behavioral Neuroscience at University of Chicago Medicine, told Medscape, “Condom use has long been a stalwart prevention mechanism, but PrEP offers superior protection and patients who are seeking PrEP are exhibiting agency and informed risk mitigation…When a patient is seeking additional protection, it is less about what is the right way to experience a sexual relationship, and more about what is the right way to be safe from HIV.”
Although this study has a number of limitations, including the fact that it is based on a controlled and hypothetical scenario and study participants are still medical students not yet licensed to prescribe, its results have important implications: It underscores the need to train clinicians to recognize and set aside their own social biases during clinical interactions.
Bunting suggested that provider training should support clinicians to evaluate patient requests in a nonjudgmental, pragmatic, and realistic manner appropriately reflecting patient informed agency and knowledge of their own risk factors.
And Marcus concurred, noting that standardizing the delivery of PrEP through a screening algorithm presents an alternative pathway for eliminating the role of stigmatizing clinician biases and working toward equitable access to PrEP.
This study was supported by unrestricted research funding from Gilead Sciences. The funder had no input into research design, implementation, analysis, interpretation, or publication decisions. Co-author Brian A. Feinstein’s time was supported by a grant from NIDA. No additional funding was received to support this research.
J Acquir Immune Defic Syndr. Published online August 19, 2022. Full text
Katie D. Schenk, PhD @skibird613 is an infectious disease epidemiologist based in Washington, DC.
Source: Read Full Article