The immune system’s double agents

A new Tel Aviv University study examined for the first time the development of a glioblastoma cancerous tumor in animal models with a normal immune system, in order to best simulate the development of the tumor in humans. The findings of the study showed that there are immune system cells that, despite the fact that their primary function is to attack and kill the cancer cells, actually act as “double agents” that increase and intensify the aggressiveness and threat of the tumor.
The study was led by Dr. Dinorah Friedmann-Morvinski of the George S. Wise Faculty of Life Sciences and Sagol School of Neuroscience, and her Ph.D. student and Prerna Magod Also participating in the study were Dr. Liat Rousso-Noori and Ignacio Mastandrea, also from the Faculty of Life Sciences, as well as other researchers from the Sackler Faculty of Medicine at Tel Aviv University and the Weizmann Institute of Science. The study was published in Cell Reports.
Glioblastoma is the most common type of brain cancer, and one of the most violent and deadly cancers in humans; the average life expectancy of glioblastoma patients is 12 to 15 months from the moment of detection. The researchers explain that usually, the scientific monitoring of the development of the cancerous tumor in animal models is carried out without an active immune system, in order to enable the absorption and growth of cancer cells in the body. The disadvantage of this commonly-used model lies in the fact that the immune system either does not exist or does not function properly, which prevents researchers from monitoring the interaction between it and the tumor cells.
The study, which was conducted in Dr. Friedmann-Morvinski’s laboratory, used a model that examined the development of cancer cells in animal models with functioning immune systems. This allowed the cancer to grow gradually, to the point of the development of a massive tumor, which enabled the close monitoring of its development, and throughout the process, of the interaction between the cancer cells and different immune system cells.
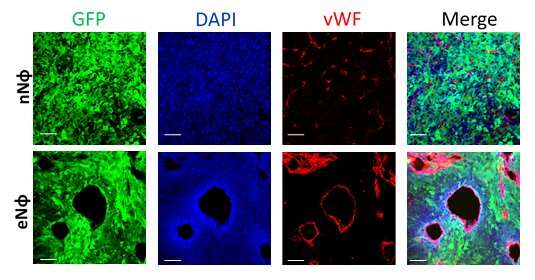
In the study, the researchers found that cells called neutrophils play a critical role in interacting with the cancerous growth. Neutrophils are immune system cells that originate in the bone marrow, and whose purpose is to “swallow” or kill bacteria and fungi and fight the infections caused by them. “Neutrophils are the front-line soldiers of the immune system,” says Dr. Friedmann-Morvinski. “When a tumor begins to develop, the neutrophils are among the first to mobilize and attack it in order to eliminate it.”
The researchers also found that the neutrophils remain in close proximity to the tumor throughout its development, and are continuously and consistently recruited from the bone marrow. The surprising thing that was discovered during this study is that the neutrophils “change sides:” Whereas at first, with the onset of the initial tumor, the neutrophils fight it, over time the neutrophils recruited to the cancerous area begin to support its development.
Dr. Friedmann-Morvinski says that “we learned that the neutrophils actually change their role. They are mobilized by the tumor itself, and from being anti-cancerous, become pro-cancerous; as a result, they aggravate the damage that the tumor itself creates.”
Moreover, the researchers found that the process by which the neutrophils change their properties can take place remotely, even before they progress towards the tumor itself.
“The study showed that the change in the properties of neutrophils takes place in the bone marrow itself—where there is no tumor at all: the cancerous tumor is located only in the brain, and from there it succeeds in changing the properties of the cells it recruits,” adds Dr. Friedmann-Morvinski. “The new findings of this study may also shed light on immunotherapeutic therapies, which have been gaining a lot of momentum in recent years. In one type of immunotherapy treatment, T cells are removed from the patient’s body, processed, and returned to the body with increased healing abilities. One of the major problems today is that even these cells that have been sent to heal are suppressed and their actions stifled. If we know how to change the interaction between neutrophils and T cells so that they are not suppressed, this will have implications for the effectiveness of immunotherapy.”
Source: Read Full Article