Understanding the variability in responses to COVID-19 illness in older adults

Since the start of the COVID-19 pandemic in December 2019, more than 200 million people have been infected with SARS-CoV-2, resulting in at least 4 million deaths, and probably closer to 7 to 9 million deaths worldwide. Interindividual clinical variability in the course of acute infection has been found to be vast, ranging from silent infection to rapid death.
Trinity researchers from the School of Medicine and Tallaght University Hospital have joined a large collaborative study, involving leading clinical research facilities from 38 countries internationally, to examine the reasons for this variability in morbidity and mortality in COVID-19 illness. The study is published in the journal Science Immunology.
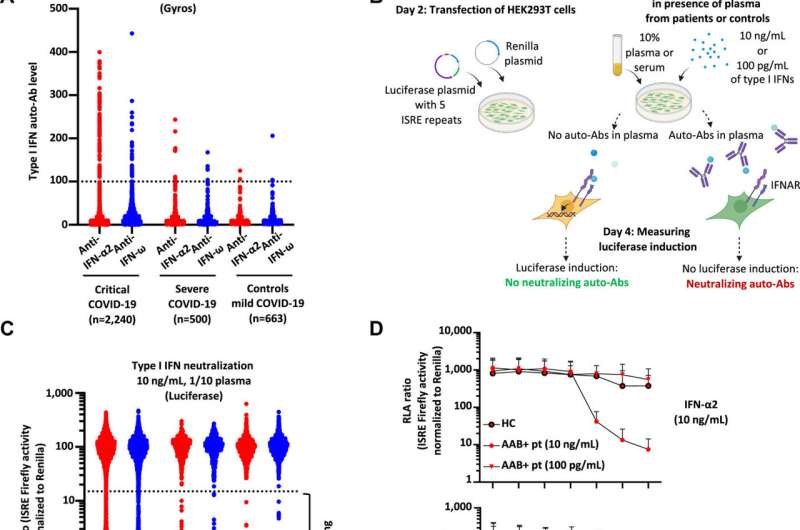
This unique study explains a new mechanism that accounts for some of the variability in COVID-19 illness. The research has found that autoantibodies—antibodies that mistakenly target and react with a person’s own tissues or organs—block a key mechanism in the antiviral immune response; the type 1 interferon response.
The type 1 interferon response is an immune mediator involved in antiviral protection and is a critical response in the body’s ability to fight viral infections. This new research shows that the autoantibodies that neutralize the interferon response, sharply increase in prevalence in patients over 60 years of age and underlie about 20% of all fatal COVID cases. Researchers believe that this may explain some of the variability that we see in COVID-19 illness in older people.
The presence of auto-antibodies in some individuals with critical COVID-19 illness was previously demonstrated by Paul Bastard (University of Paris, France) and Jean-Laurent Cassanova (Howard Hughes Medical Institute, NY, U.S.). Bastard and Cassanova have led this current collaborative study which demonstrates this key mechanism by which some individuals are more vulnerable to COVID-19 illness. These autoantibodies sharply increase with age and are present in about 4% of older adults aged >70 years of age in the general population, partially explaining why older adults are so vulnerable to severe COVID-19.
Key findings
- Auto-antibodies neutralizing type I interferons (a key immune defense mechanism) are present in 4% of adults aged 70 years or older and may account for up to 20% of COVID-19 deaths.
- Auto-antibodies are capable of neutralizing the body’s own interferon anti-viral response.
- Auto-antibodies sharply increase after the age of 70 years.
The Irish contribution to this wider global research effort came from the inclusion of older individuals which were part a larger program of research at Trinity College Dublin and Tallaght University Hospital. The NH-COVAIR project is a longitudinal investigation of COVID-19 in Irish nursing home residents, examining the relationship between frailty, Clinical outcomes, immunophenotype, and vaccine response in nursing home residents.
The inclusion of this information into the larger global study is vital as older adults, and particularly those residing in nursing homes, are frequently excluded from research based on age or medical co-morbidity. This study, by demonstrating the striking increase in these autoantibodies after 70 years of age, emphasizes the need to not only include older adults in immunology research, but the need to study the variability in immune responses in older adults and in particular in those living with frailty, such as nursing home residents. By excluding older adults from research, this could mean the opportunity for key discoveries about immune system variability is lost.
Implications for clinical care and treatment
The research presents several possibilities for clinical care and treatment of the COVID-19 illness. The identification of these auto-antibodies may inform clinicians about who is more susceptible to severe COVID-19 illness, who may benefit from early hospital admission and early treatment and who may benefit from therapy such as interferon-beta ( trials of nebulised interferon-beta are currently underway).
The Trinity team’s ongoing NH-COVAIR study, is led by Dr. Adam Dyer, Professor Seán Kennelly and Dr. Nollaig Bourke, will aim to explore these responses further over the course of the next few years. This research emphasizes the need to include older people and those with advanced levels of frailty in basic scientific research.
Professor Seán Kennelly, Consultant Physician in Geriatric and Stroke Medicine, Department of Age-related healthcare, Tallaght University Hospital and Clinical Associate Professor in Medical Gerontology, Trinity College and co-author of the study said: “This important study explains why COVID-19 can have severe clinical consequences in some people but not others. We were delighted to ensure Tallaght University Hospital and Trinity College Dublin were represented amongst this international consortium of leading clinical research institutes. We are extremely grateful for the generous support of local nursing home residents, staff, and families who participated in this study.”
Source: Read Full Article