Primitive stem cells point to new bone grafts for stubborn-to-heal fractures

Although most broken bones can be mended with a firm cast and a generous measure of tender loving care, more complicated fractures require treatments like bone grafting. Researchers at Texas A&M University have now created superior bone grafts using primitive stem cells. They found that these cells help create very fertile scaffolds needed for bone to regenerate at the site of repair.
The researchers said these grafts could be used to promote swift and precise bone healing so that patients maximally benefit from the surgical intervention.
“There are several problems that can occur with orthopedic implants, like inflammation and pain. Also, they can loosen, requiring revision surgeries that are often more complicated than the original surgery to put in the implant,” Dr. Roland Kaunas, associate professor in the Department of Biomedical Engineering and a corresponding author on the study. “So, by speeding up the bone healing process, our material can potentially reduce the number of these revision surgeries.”
The researchers have published their findings in the June issue of the journal Nature Communications.
Each year, around 600,000 people in the United States experience delayed or incomplete bone healing. For some of these cases, physicians turn to surgical procedures that involve transplanting bone tissue to the repair site. These bone grafts have generally come from two sources: the patient’s own bone from another location on the body called autografts, or highly-processed human cadaver bones.
However, both types of bone grafts have their share of drawbacks. For example, autografts require additional surgery for bone tissue extraction, increasing the recovery time for patients and sometimes, chronic pain. On the other hand, grafts derived from cadaver bone preclude the need for two surgeries, but these transplants tend to be devoid of many of the biomolecules that promote bone repair.
“Grafts from cadaver bone have some of the physical properties of bone, and even a little bit of the biological essence but they are very depleted in terms of their functionality,” said Dr. Carl Gregory, associate professor at the Texas A&M Health Science Center, also a corresponding author on the study. “What we wanted to do was engineer a bone graft where we could experimentally crank up the gears, so to speak, and make it more biologically active.”
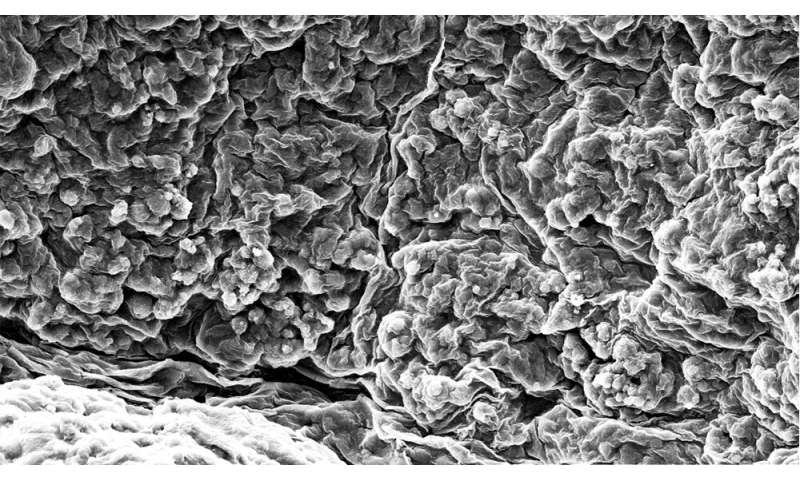
Previous studies have shown that stem cells, particularly a type called mesenchymal stem cells, can be used to produce bone grafts that are biologically active. In particular, these cells convert to bone cells that produce the materials required to make a scaffolding, or the extracellular matrix, that bones need for their growth and survival.
https://youtube.com/watch?v=0vkhrtrN-as%3Fcolor%3Dwhite
However, these stem cells are usually extracted from the marrow of an adult bone and are, as a result, older. Their age affects the cells’ ability to divide and produce more of the precious extracellular matrix, Kaunas said.
To circumvent this problem, the researchers turned to the cellular ancestors of mesenchymal stem cells, called pluripotent stem cells. Unlike adult mesenchymal cells that have a relatively short lifetime, they noted that these primitive cells can keep proliferating, thereby creating an unlimited supply of mesenchymal stem cells needed to make the extracellular matrix for bone grafts. They added that pluripotent cells can be made by genetically reprogramming donated adult cells.
When the researchers experimentally induced the pluripotent stem cells to make brand new mesenchymal stem cells, they were able to generate an extracellular matrix that was far more biologically active compared to that generated by mesenchymal cells obtained from adult bone.
“Our materials were not just enriched in the biological molecules that are required to make the chunky part of bone tissue but also growth factors that drive blood vessel formation,” said Gregory.
To test the efficacy of their scaffolding material as a bone graft, they then carefully extracted and purified the enriched extracellular matrix and then implanted it at a site of bone defects. Upon examining the status of bone repair in a few weeks, they found that their pluripotent stem-cell-derived matrix was five to sixfold more effective than the best FDA-approved graft stimulator.
“Bone repair assays using the gold standard of grafts, like those administered with the powerful bone growth stimulator called bone morphogenic protein-2, can take about eight weeks, but we were getting complete healing in four weeks,” said Gregory. “So, under these conditions, our material surpassed the efficacy of bone morphogenic protein-2 by a longshot, indicating that it is a vast improvement of current bone repair technologies.”
The researchers also said that from a clinical standpoint, the grafts can be incorporated into numerous engineered implants, such as 3-D-printed implants or metal screws, so that these parts integrate better with the surrounding bone. They also noted that the bone grafts will also be easier to produce and hence are advantageous from a manufacturing standpoint.
Source: Read Full Article