Established drug for symptoms of angina pectoris also protects vascular system
A drug used in the clinical treatment of angina symptoms also has an anti-inflammatory effect and reduces atherosclerotic plaques in blood vessels—thereby reducing the risk of heart attack or stroke. The study, led by MedUni Vienna and including access to data from Harvard Medical School, has now been published in the Proceedings of the National Academy of Sciences.
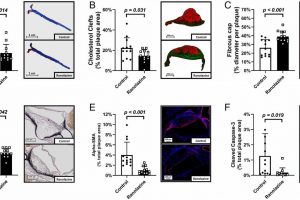
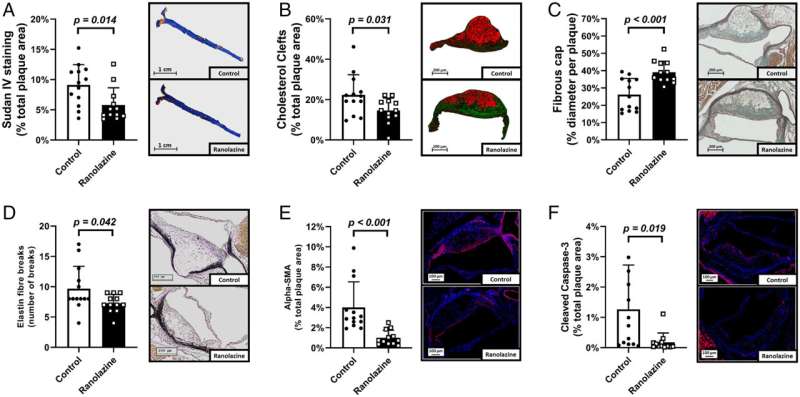
The complications of atherosclerosis—heart attack and stroke—are the leading causes of death in Europe and the United States. In recent years, it has been shown that chronic inflammation in the arteries leads to the formation and progression of atherosclerotic plaques (deposits in the blood vessels). The MedUni Vienna research group led by Walter Speidl (Department of Medicine II, Division of Cardiology) and Philipp Hohensinner (Center for Biomedical Research) has now demonstrated for the first time that a reduction in intracellular sodium concentration inhibits the important inflammatory modulator NF-kappa-B. The drug ranolazine is a long-established drug used to relieve the symptoms of angina pectoris. However, it also inhibits the uptake of sodium into cells.
Johann Wojta, Head of the Cardiology Research Laboratory at the Medical University of Vienna, and co-author of the study explains, “In this publication, we used research involving cell culture, animal models and a large-scale human study to identify a new mechanism for inhibiting inflammation in atherosclerosis. We now have evidence that an established drug not only combats the symptoms of angina but can also reduce the risk of heart attack and stroke.”
Using data provided by Harvard Medical School, this anti-inflammatory effect was demonstrated in 6,500 patients who had suffered myocardial infarction. It was found that treatment with ranolazine results in lower levels of the inflammatory and cardiovascular risk marker “high-sensitivity C-reactive protein” compared to placebo.
Source: Read Full Article